Gene editing itself has truly just been the start of the modern biotechnological revolution. As time has passed, the nuance of capability with tools like CRISPR has evolved to not only be more precise, but to also have additional options beyond just additions or deletions of genes. New versions have included things like inducing point mutations and altering the epigenome for gene silencing, enhancement, and more.
For the medical field, dozens of experiments are underway around the world on any number of diseases in the hopes of preventing them. Cancer can potentially be cured by having the immune system recognize the cancer cells as harmful by changing receptors on their surface. A similar but opposite mechanism can be used on cells to change the receptor that HIV binds to, making said people immune to the virus. Until it mutates again, of course.
CRISPR has been at the forefront of these challenges due to it offering a simple, yet multifaceted mechanism for changing genes and thus protein expression in all living organisms. The usual method of delivery of the CRISPR complex has been either the use of plasmids that have the coded information for making the system into them or by making the system in vitro ahead of time and delivering them into cells, usually through a neutral viral vector.
The Effectiveness of RNPs
A third method that has gained popularity has been the use of a ribonucleoprotein (RNP) complex. This is where CRISPR and its guide RNAs are assembled and activated ahead of time and then moved into cells through options like microinjection, electroporation, or other such mechanical processes. These RNPs are set to start their jobs immediately once they enter a cell, unlike other CRISPR delivery methods, and straight away begin their coded instructions.
Because they are turned on directly, the livespan of these CRISPR RNPs is short, which has its upsides and downsides. The time limit means that the risk of off-target changes occurring is practically nonexistent and it is effective at changing all of the target cells immediately, reducing any time period of mosaicism where some cells are modified and some aren’t.
Since these RNPs are delivered sans additional information, they are not very useful for insertion of foreign DNA, but instead are best for creating point mutations at desired locations. A side benefit of not using plasmids is that one form of the innate immune system activated by cyclic GMP-AMP synthase, a DNA sensor in the cytosol, does not recognize viral invasion when it comes to RNPs. So that’s one big problem when it comes to immune responses dealt with.
There is another concern to note however. The guide RNAs (gRNA or sgRNA) complexed with CRISPR are usually encoded into being in vitro with the use of bacteriophage polymerases like those from T7 or SP6. Being in vitro-transcribed (IVT) by these viral polymerases creates a unique addition to their structure, a triphosphate group at the 5’ (front) end of the RNA sequence. The problem with this addon is that it does activate another part of the innate cellular immune system, as the gRNA is seen as a “non-self RNA” likely from a virus. This in turn causes the mobilization of antiviral effector proteins like DDX58, OAS2, and PKR.
Confirming The Immune Response
Since this is yet another primary obstacle to medical usage of CRISPR gene editing in human cells, researchers from several universities and research centers in South Korea decided to try and tackle the RNP response with a basic, yet efficient solution.
The first experimental test they ran was to see whether these IVT guide RNAs also caused an immune response in cultured human cells. T7 polymerase was used to synthesize them and they were complexed with CRISPR Cas9 before being introduced into HeLa cells using lipofection, which is a method that uses vesicles called liposomes that are able to merge with the cell wall and release their contents to the interior.
As expected, the gRNAs caused a 1000-fold mRNA increase in immune response genes and a 200-fold increase in immune protein production like DDX58 and OAS2. When the Cas9 was tested by itself, it did not have a response, but the gRNAs by themselves did, confirming that it is the guide RNAs that are causing immune system activation. Another effect the immune response had was cytotoxicity, where the cells dealt with the perceived viral infection by causing cell death, resulting in 80% of the exposed cells expiring.
A Simple Solution
Next, the gRNAs were chemically introduced to phosphatases from calf intestines that changed their 5’ triphosphate group into a 5’ hydroxylated (OH) group. The desired result of no immune response was observed once these gRNAs were used, including no cytotoxic response.
For both forms of the guide RNAs, their editing capabilities with the Cas9 complex was measured and both saw equal efficiency, showing that the immune response itself had no effect on the ability of CRISPR to gene edit per its instructions. However, the cell death in the prior version did make the editing inconsequential, since modified genetics is meaningless if the cell dies.
While their change to the guide RNAs worked, the scientists wanted to know more about what specifically in the immune response was sensing that 5’ triphosphate group. They hypothesized that it might be the DDX58 gene that was acting as the immune sensor in this case. Thus, they used a DDX58-knockout cell without the gene to test this and, voila, even the original gRNAs worked fine with no immune response, confirming their suspicions.
The Active Immune Cell
A secondary series of experiments worked on the same topic with another popular CRISPR editor in the form of Cas12 (Cpf1). The same tests with their RNPs, gRNAs, and other functionality was conducted with the same results as with Cas9. So this can be a solution for both, and potentially all, CRISPR systems to get around immune responses.
The final test was to see if the same thing worked in immune cells themselves, such as CD4+ T cells that were freshly donated from volunteers for the experiment. A Cas9 RNP was used and introduced via electroporation and made to target the CCR5 gene that is an essential receptor for HIV infection. The viability and health of the cells were measured via ATP levels.
As before, the 5’ triphosphate gRNAs caused an immune response and the 5’ OH gRNAs did not. Interestingly, when it came to the desired mutation in the CCR5 gene, the 5’ OH gRNAs had a slightly higher success rate beyond the standard deviation (92% vs 80%). So, in healthy immune cells, the immune response to perceived viral infection does also slightly inhibit CRISPR’s gene editing systems.
The Next Step For Medicine
Overall, this series of experiments from South Korean researchers has provided a viable alternative method to dealing with immune system response for CRISPR RNP usage. The change of the gRNAs to an OH state is not difficult to do either, making it a simple additional step for medical usage of CRISPR in treating cancer, HIV, or other diseases.
Targeted cell therapy can now be considered a viable reality, so long as subsequent testing by other research groups comes up with the same results. With the last big obstacle passed, we may be soon seeing CRISPR treatments over the next decade for any number of problems. Hopefully no new issues or roadblocks will emerge to stop their success.
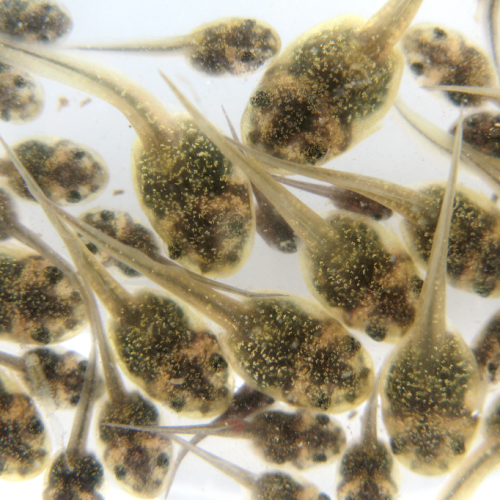
Photo CCs: HIV-budding-Color from Wikimedia Commons