With the great strides and advances in medicine that have been brought to the stage in the past several decades and especially in the past ten years, there has been a shift in focus and perspective in the pharmacological community. Previously, the task had been to develop medicines to treat conditions big and small or, for those still incurable diseases, to stymie the symptoms caused by them. That remains an ongoing area of research and likely will for many years to come, if not forever, but there has been a new group of scientists and their experiments that have become the primary talk of pharmacological studies.
The field they have helped create is known as pharmacogenomics (or pharmacogenetics, the terms are interchangeable), the study of genetics and tailoring pharmaceuticals for the individual. As a form of personalized medicine, the research into genetic impacts on the effectiveness of medications has only really become a reality in recent years alongside the expansion of genetic machinery that is effective and low-cost, comparatively. Now that a full genome sequencing is available for the average person, their genetic risks and variances can be unearthed and qualified, allowing for medicines to be chosen based on those results.
But even though the true ability to combine such information has only come in modern times, the idea and attempted use of pharmacogenomics goes much further back. To give an example, the term itself was made as an initial neologism in 1959 by the famed German human geneticist Friedrich Vogel, who helped reclaim the positive nature of the field of genetics and reformed it after the atrocities committed by the Nazis in the name of science. The meaning of the term back then holds largely the same today, describing the genetic differences that cause the effects of a pharmaceutical to vary in an individual, whether speaking of negative side effects or positive therapeutic effects.
The Individualized Nature of Pharmacogenomics
It was the sequencing of the human genome in 2002, the first true draft copy at least, that kicked things into high gear. The outlook back at the time was incredibly optimistic and some viewed the medical community as being able to unravel the innate genetic nature of disease within a decade. Of course, it didn’t work out like that. As with many things in science and especially when it comes to genetics, there was far more complexity than expected. The pharmacological connection to genetics was not a simple toggle switch between an on or off position. The real nature of life is a myriad of interlocked genes controlling a cascade of response factors, with any change to a single one altering all the others as well.
Advancements have still been made regardless, with clinical application of the research coming online since then. These improvements have primarily been focused around those suffering from extreme diseases, like cancer, stroke, epilepsy, or diabetes. Mood disorders especially, since they by their very nature involve changes to processing of neural chemicals, have seen a scientific spotlight placed upon them with this research.
Personalized Medicine Among Populations
It needs to be reiterated though that while some general breakthroughs have been made, the majority of this experimentation has proven that there is no “one size fits all” treatment, as it is also someone’s personal genetics that interacts with their condition to form their unique relationship with pharmaceutical responses. This sort of targeted drug therapy based on genetic triggers required a personalized approach, as we are learning that there are certain genes that, if not accounted for, can result in causing far more harm to a patient than good.
An area where the advancement in swift genetic testing and, with high end enough technology, rapid sequencing itself proves most useful is in the intensive care unit (ICU). When dealing with immediate crises from injuries, diseases, or other such conditions, knowing what medication is safe or proper to use is paramount and this goes far beyond just dealing with allergenic responses. A person’s genetics can result in them metabolizing common compounds slower or differently than the majority of the population, cutting the effectiveness of the medication and requiring a completely different treatment regimen.
This has been found to be especially true for people from disparate regions of the world, where long-standing genetic regions may have developed unique polymorphisms in their genome in response to things like diet over generations. Over decades and a long line of individuals, small changes in habits, lifestyle, and many other factors can shape a population’s genetics so that they process vitamins, minerals, and medicinal compounds in different ways. Therefore, the study of population genetics, as just mentioned, is another field deeply entwined with pharmacogenomics.
Genetic Drug Responses
Before moving on to more specific science, it would be remiss not to give a general overview of the kinds of drug responses that genetics can manipulate. While a list could be made of particular factors, that wouldn’t be very helpful to readers, so let’s keep things broad.
The first and most obvious group are the drug-metabolizing enzymes, the proteins that actually break down drugs that are introduced into our systems. Depending on their functionality, they can lead to both a reduction in effect of a drug as compared to an average person or an increase in that effect. A lot of the adverse reactions seen from drugs come about from genetic alterations to these enzymes.
People with two copies of the gene coding for the enzyme, so those who are homozygous, are able to metabolize said drug easily. Heterozygous individuals would obviously have a slower metabolic breakdown speed and those homozygous against the gene would be almost entirely incapable of properly utilizing a drug as intended. This doesn’t mean they have no symptoms resulting from drug consumption, as it is possible for their systems to, when unable to follow the normal metabolic route, try and break down the drugs through another pathway. Such a change can result in toxic compounds being made or other undesired effects. The interplay of different enzymatic pathways is highly important to understanding how drugs are used, but they are also some of the most difficult biochemical and genetic systems to learn about.
Just as relevant are the transport proteins that move the active components of a drug to the proper cellular (or extracellular) location for use. The speed at which this transportation happens, among other forms of efficiency, determine the rate of absorption of a drug, whether it is distributed to the appropriate bodily locations, and the rate of excretion from the body. Every step of that chain can alter how a drug’s effects are perceived by the body on a macro scale. If drugs are not transported at the correct rate, they could build up in the tissues and once again cause toxicity symptoms.
The last major form of genetic manipulation are the cellular receptors that recognize and bind to the drug compounds. The genes that control the formation of these receptors can be very easily altered so that they are no longer capable of recognizing the relevant molecules and, in some rare and undesirable cases, can recognize completely different compounds that then cause adverse effects. These genes can also be up or downregulated epigenetically, which will change the amount of response an individual has to a medication.
Collaborative Projects For Genome Breakdown
In order to scan across populations and to find the individual genes relevant to such research across all of the human genomes out there, research groups have taken to using genomewide association studies (GWAS) to conduct these investigations. Previously, these had only been done to look for disease factors and physical trait differentiation, so the amount of data available on drug response genetics was severely lacking. Out of the available 2,431 GWAS experiments in the literature, only 182 were found to have anything to do with pharmacological responses.
A collaboration was instituted in 2008 between the National Institute of Health’s Pharmacogenomics Research Network (PGRN) and Japan’s RIKEN Center to fund and conduct more GWAS experiments in this area. Annual meetings allow results from such funded projects to be presented and discussed, along with new proposals to be given for consideration. Currently, out of the 41 independent projects being supported, 19 have a focus on anti-cancer drugs and how to detect and limit their toxicity in the body. Efficacy genes can greatly change how well the treatments are taken, with one study even finding special gene variants in Asian populations that made them susceptible to a drug-induced form of thrombocytopenia.
Luckily, there is some advantage to be taken from the knowledge gathered in other GWAS studies, as understanding the workings of a disease and the biological pathways by which diseases harm the body, this can also help in creating more targeted treatments. The PGRN-RIKEN meeting in 2016 acknowledged, however, that there is still more data that needs to be collected from both a wider cohort of people as a generalized population study and more specific studies from multiple regions to find more individualized genetic variances.
Another organization recently formed, this time at the behest of the US Food and Drug Administration was the Clinical Pharmacogenetics Implementation Consortium (CPIC), in order to review drug submissions and provide guidelines for packaging information and usage requirements. By 2016, around 18 guidelines had been made for the major drug classes to help the public use them appropriately and to list those that might be at risk when taking such medications.
The National Institutes of Health saw fit in 2013 to fund another group termed the Implementing GeNomics In praTticE (IGNITE) network to help more directly develop new drugs and to make models for implementing, per their name, genomic medicine. The corresponding universities working with IGNITE have largely focused on the main genes involved with bioprocessing of the drug clopidogrel.
Since the drug is used to reduce the risk of heart disease and stroke and is commonly employed after heart surgeries, the genetics behind biologically manipulating it are important. Between 30 and 65% of people, depending on racial background, have an inactive form of the CYP2C19 gene. This non-functional gene reduces the rate of integrating the medicine and dramatically increases the risk of adverse heart-related conditions. Thus, the guidelines that have been suggested require testing for the gene and alternative therapies if the patient has the inactive form.
Similar studies elsewhere have found other heart-related drug responses, like with the medicine BiDil. This was found to be highly effective in those with recent African ancestry, but far less on other racial backgrounds, especially Caucasians. The Veterans Administration Cooperative Study was used to help test for this and other drug responses between racial groups in the early 1980’s as one of the first proper population genetics studies of its kind.
Before too much faith is placed in this topic, it should be pointed out that racial ancestry is not as simple as geographical location. Some unique genetic groups are both too specific for generic racial terms to cover them and, in other cases, too spread out for geography to really be helpful when classifying population genetics for pharmaceuticals. It is also possible for individual genes to be passed on even through the thinnest of ancestries, making it difficult for people in current times to truly know what gene components they have without a full sequencing being done.
Thus, it can be an oversimplification to group drug responses to general race categories. Many studies do so for convenience, but researchers in pharmacogenomics have to be careful not to make wrong conclusions that don’t follow the evidence just because they don’t match up to the racial categories our society has created.
The Subfields of Pharmacogenomics
Now that we’ve covered the basics of this field of study and an overview of projects being undertaken over the past few decades, we can now go into specifics related to the subfields of pharmacogenomics and the areas of research that are being spotlighted. These cover big, well-known diseases, as you might expect, since finding out the genetic connection to pharmaceuticals with these can pave the way for better usage for smaller diseases.
Psychiatric Pharmacogenomics
An expansive and largely untapped sub-region of pharmacogenomics is the use of genetic research to treat mental and mood disorders. It is quite obvious to see that this is one place where you would expect the biggest results to be happening, due to pharmaceuticals being one of the few options for treating such conditions and restoring “normal” neurological function. But it hasn’t been that easy.
A difference between oncological diseases and those found in psychiatrics is that the latter doesn’t always have clearcut conditions to study and more often are general symptoms combined into a disorder. That makes finding genetic causes for the conditions complicated at best. So standardizing research in this region cannot be done in a simple manner and genetic influence must often be as general as the conditions they are purported to be connected to.
That doesn’t stop commercial genetic tests from being made, with panels for different drugs types that patients are grouped into based on their metabolizing rate for each drug. Some of these even add in information about the transporters and receptors mentioned in a prior section. The sad part is that many of these commercial tests end up to not just be ineffective, but even complete bunk, as they make claims about genetic associations that, as of yet, there is no scientific evidence backing their connection to these disorders.
These fake results match the sad history of mood disorder research. The first true breakthrough started in 1987 with a paper in Nature stating to have found a genetic marker in the chromosomes believed to be linked to bipolar disorder. It was huge news at the time, because there had been concerned rumbles that the genetic basis for mental conditions would never be nailed down.
Unfortunately, those fears were cemented even stronger when repeat tests by other groups over the next few years were unable to replicate the results. This has happened repeatedly in the decades since, with a big study announcing to have found a mood disorder link and then the results being found to be insignificant after inspection of the data. By 2008 even, a systematic review of the literature found no reliable signal markers in the genome, due to the lack of successful replication of the dozens of claimed studies in the past.
It didn’t help that at the same time as that review was being published, the largest ever patient study of 3,000 people with bipolar disorder was completed and found absolutely no genetic markers connecting any of them to the disorder. This led to a huge drop in funding as it was assumed by government agencies that there was just nothing to find if so much effort over decades had not found a single genetic source. If they did exist, they were clearly too convoluted to pick out of the mess of the genome with the current technology of the time.
That didn’t stop psychiatrists in the field from trying, but it did make them reevaluate their aims. With success being reported in other complex diseases like diabetes, the methods used there worked to inform researchers on how they need to conduct a proper mood disorder study. What they concluded is that it needed to be big, far bigger than any such study they had done before. Not with 3,000 people, but 100,000. And they need to look for not a single or handful of genes, but for any gene variances across the genome that caused even a slight increase in the risk odds for the condition.
Per the findings in other medical fields, it was expected that dozens of genes individually contributed a small amount of risk to developing a psychiatric condition, thus making it almost (but not quite) impossible to tease out the contributors. It was this realization that completely revolutionized the psychiatric field involved in genetics. A Psychiatric GWAS Consortium was made to do genomewide studies on populations around the world and to collect as many DNA samples as possible from sufferers of these conditions.
Thanks to this new method of research, the first true gene variant for bipolar disorder, named CACNA1C, was found. Other disorders were able to replicate these achievements, with depressive disorder scientists finding 15 genes with strong indications of connection. It has been confirmed that study samples in the realm of 100,000 people are required to be able to find the minimal contributions from each gene.
But the genes interacting with the disorders are only one half of pharmacogenomics, the other half, of course, is genes that change interactions with medications. For generalized conditions, the most promising research to date involves the drug carbamazepine, a neuropathic pain medication used for a lot of states like with schizophrenia and bipolar disorder. It even sees usage beyond just mental conditions and into other brain and nervous system issues like with epilepsy and seizures.
While side effects are uncommon, the rare instances can be quite severe, causing two dangerous skin conditions known as Stevens-Johnson syndrome and toxic epidermal necrolysis. Those of Asian descent were found to have a higher likelihood of having a HLA-B gene variant different from the rest of the population and which causes those side effects under carbamazepine treatment.
The HLA-B gene can be found associating with the drug clozapine too where it creates a blood-related side effect that reduces neutrophil numbers named clozapine-induced agranulocytosis (CIA)/clozapine-induced granulocytopenia. Since the drug is a treatment for schizophrenia, the question is whether to discontinue practically the only source of relief for the condition or to continue with the drug treatment even though the side effect condition could end up being life-threatening. Being able to predict this side effect in advance would be of incredible use for medical professionals.
Epilepsy Pharmacogenomics
Due to the high amounts of medication involved in its treatment, epilepsy has been a focal point for pharmacogenomics research as a method to find out the activity of several multi-purpose drugs. The kaleidoscope of epilepsy types and subsequent medicine changes makes the use of antiepileptic drugs complicated, requiring a large amount of modification over the course of treatment.
Since these drugs also have well known and often severe adverse effects from consumption, being able to mitigate or minimize the expression of these through genetic sequencing to find the best possible medication is the preferable option. With over 30% of all epilepsy patients having to deal with some kind of adverse reaction, gene-drug interactions are a topic of study for most epilepsy scientists and doctors.
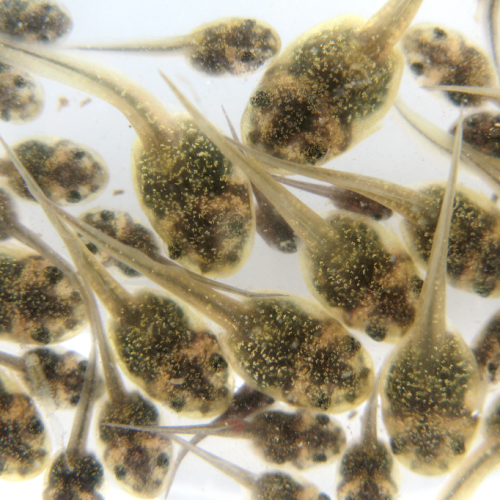
What do we know thus far? Well, the basic information is that antiepileptic drugs are commonly processed through a group of enzymes known as the cytochrome P450 (CYP) family. The genes controlling this family have several variants, causing fluctuations in metabolism and enzymatic pathway usage. If the wrong pathway is genetically favored, this can lead to the production of toxic compounds in the body.
Phenytoin is a routine antiseizure drug used for epilepsy, heart arrhythmia, and sometimes pain involving the nervous system. It is 90% processed by the CYP2C9 gene, whose variants determine its speed of breakdown. People with the variant have to be given significantly lower doses due to their slow metabolic process, where too high a dose can cause it to linger in the body and become a neurotoxin.
Clusters of single nucleotide polymorphisms (a single mutation) in this gene were found in significant quantities within populations in Taiwan. These mutations commonly resulted in adverse skin reactions to phenytoin, The biochemical reason behind why this gene mutation causes this has yet to be uncovered.
A separate CYP gene called CYP2C19 was found to interact negatively with the drugs clobazam and its metabolite N-desmethylclobazam (N-clobazam), which act as anticonvulsants and antianxiety medicines. The exact results have yet to be investigated, so little beyond the gene-drug connection is known and that the gene variant was found in Asian populations.
Several other classes of drugs have been found to interact with both of the aforementioned CYP genes, though the results have yet to be replicated and further explained. Sadly, most epileptic research of the needed genomewide, high sample population type is severely lacking and has yet to be conducted.
The Pharmacogenomics of Cancer
When it comes to cancer, it’s pretty plain that the many forms of it are the defacto main topic of disease research, the one that so much funding is spent on. And, unlike with how it is often portrayed, cancer is so varied that sometimes it is even the case already that a patient’s personal version of cancer is unique and must be treated as such. This places it firmly in the realm and reach of pharmacogenomics, but also raises the stakes. For, while generalized genetics could be found in some cases with other diseases, at best, cancer research can only find genetics that pertain to a single kind of cancer. And that’s only with the very best results from a wide-scale study.
Breast cancer continues to be one of the prominent cancers affecting the human race, with it being a top five cause of death for women around the world, especially in countries without adequate diagnosis and treatment facilities available. Genetic research, therefore, has been a mainstay of assessing risk far ahead of time for developing this type of cancer (and for many others). Treatment beyond chemotherapy, however, relies on precise understanding of drug impact, since so many of the drugs used herein can have fatal side effects if used inappropriately.
For liver breakdown of these drugs, the same cytochrome P450 enzymes play a role as with epilepsy. Tamoxifen is a decades old generic medication for breast cancers that is processed by the enzyme CYP2D6 into metabolites that block and restrict the activity of estrogen receptors, thus inhibiting the estrogen response genes that play a role in developing breast cancer cells. But CYP2D6 has 46 gene variants to its name, many of which just render the enzyme completely nonfunctional. This in turn makes tamoxifen a completely useless drug for patients with these gene variants, something that would be very important to know before commencing treatment.
It is additionally possible for gene variants to alter the toxic byproduct or end product from drug metabolism, changing from one expected pathway to another and changing the medical response needed to keep toxicity levels down. This is the case for the drug Irinotecan, used for multiple cancer phenotypes. Hydrolysis processes in liver cells transform this drug into another active form named SN-38 that is then metabolized by enzymes from the gene UGT1A1 so the metabolite can block DNA replication in cancerous cells. Polymorphisms in this gene, however, can drastically change the final toxic leftovers, requiring vigilance and biochemical testing when taking this medicine.
A cross purpose gene sequence in the ABC transporter protein family called ABC11 is strongly associated with breast cancer cells in wild type sequences. It has been found to decrease cellular drug concentrations when medications are attempted to deal with the cancer cells. Worse still, variants on the gene are able to confer breast cancer cell drug resistance to several other classes of drugs used in treatments.
For other types of cancer, such as pancreatic cancer, particular gene mutations in adult cells determine the kind of cancer cell they turn into and how aggressive the spread is. A progressivity index is used to measure this based on what gene regulations are manipulated. Inherited gene conditions may also cause other effects, like inflammation and the spread of cancer cells to other organs.
Controlling for the spread of cancer relates directly to the drugs being utilized, as misuse of a drug on a patient with the wrong genetic phenotype can cause more harm than good. Especially when dealing with chemotherapy medicines that already have damaging side effects in order to try and wipe out cancerous cells. A narrow line must be walked in order to reach the desired chance of curing an individual’s form of cancer, made all the more convoluted by how the body often recognizes cancer cells, or is made to recognize them, as a functioning part of the human system.
The Future of Pharmacogenomics
If anything has been made clear from the discussion in this article, I hope that it is that the options for using pharmacogenomics are just at the precipice of being explored. There is so much we don’t know about gene-drug interactions and many things we couldn’t know until next generation sequencing technologies made genome sequencing and mapping affordable enough for personalized medicine to be viable.
Even the studies already completed only give indications and suggestions of gene interactions, but they will need to be corroborated by further research. But it is plain to see that the true development of individualized medicine tailored to one’s genetic profile will not only improve our ability to keep ourselves healthy, but will also reduce the risk of some medications. Lives that would otherwise be lost can be saved.
This really becomes a field that, to do it proper justice, would need to be revisited ten years from now, once true progress has been made toward understanding of these interactions and diseases. I hope that this article has managed to tantalize about what limits of medical science we are just beginning to unearth and where it might take us.
References
1. O’Donnell, P. H., & Ratain, M. J. (2015). Chapter: Pharmacogenomics. The Molecular Basis of Cancer (4th ed.). doi:10.1016/B978-1-4557-4066-6.00049-4
2. Rollinson, V., Turner, R. M. & Pirmohamed, M. (Oct 2017) Pharmacogenomics: an overview. Clinical Pharmacist 9 (10). doi: 10.1211/CP.2017.20203640
3. Sadee, W. (Aug 2017) Personalized Therapeutics and Pharmacogenomics: Integral to Personalized Health Care. Pharmaceutical Research 34 (8), 1535–1538. doi: 10.1007/s11095-017-2170-y
4. Mackenzie, M. & Hall, R. (Jan 2017) Pharmacogenomics and pharmacogenetics for the intensive care unit: a narrative review. Canadian Journal of Anesthesia 64 (1), 45–64. doi: 10.1007/s12630-016-0748-1
5. Yee, S. W. et al. (Nov 2016) Genomewide Association Studies in Pharmacogenomics: Meeting Report of the NIH Pharmacogenomics Research Network-RIKEN (PGRN-RIKEN) Collaboration. Clinical Pharmacology & Therapeutics 100 (5), 423–426. doi: 10.1002/cpt.405
6. Cavallari, L. H. (May 2017). The IGNITE Pharmacogenetics Working Group: An Opportunity for Building Evidence with Pharmacogenetic Implementation in a Real-World Setting. Clinical and Translational Science, 10 (3), 143-146. doi:10.1111/cts.12456
7. Lakiotaki, K. et al. (Aug 2017) Exploring public genomics data for population pharmacogenomics. Plos One 12 (8). doi: 10.1371/journal.pone.0182138
8. Hirschtritt, M. E., Besterman, A. D. & Ross, D. A. (Oct 2016) Psychiatric Pharmacogenomics: How Close Are We? Biological Psychiatry 80 (8). doi: 10.1016/j.biopsych.2016.08.007
9. Serretti, A. (2017) Genetics and pharmacogenetics of mood disorders. Psychiatria Polska 51 (2), 197–203. doi: 10.12740/PP/68914
10. Verbelen, M., Weale, M. E. & Lewis, C. M. (Jun 2017) Cost-effectiveness of pharmacogenetic-guided treatment: are we there yet? The Pharmacogenomics Journal 17, 395–402. doi: 10.1038/tpj.2017.21
11. Balestrini, S. & Sisodiya, S. M. (Jan 2017) Pharmacogenomics in epilepsy. Neuroscience Letters. doi:10.1016/j.neulet.2017.01.014
12. Serra, M. & Hattinger, C. M. (May 2016) The pharmacogenomics of osteosarcoma. The Pharmacogenomics Journal 17 (1), 11–20. doi: 10.1038/tpj.2016.45
13. Dornblaser, E. K., Worby, C. P., & Brazeau, D. A. (2017). Chapter: Pharmacogenomics and Cardiovascular Disease. Emerging Applications, Perspectives, and Discoveries in Cardiovascular Research, pp. 161-169. Retrieved December 14, 2017, from https://books.google.com/books?hl=en&lr=&id=GYMJDgAAQBAJ&oi=fnd&pg=PA161
14. Hossain, A., Siddique, A. B., & Auniq, R. B. (Jul 2017). Pharmacogenetics: Focus on Breast Cancer Treatment. Journal of Neoplasm, 2 (2), 1-3. Retrieved December 14, 2017.
15. Bereshneh, A. H., Morshedi, F., Hematyar, M., Kaki, A., & Garshasbi, M. (Feb 2017). Pharmacogenetics and Personalized Medicine in Pancreatic Cancer. Acta Medica Iranica, 55 (3), 194-199. Retrieved December 14, 2017, from http://acta.tums.ac.ir/index.php/acta/article/viewFile/6216/4916
Photo CCs: VariousPills from Wikimedia Commons