The cellular processes of aging are complicated and varied. There are both genetic and mechanical components that all have an ultimate effect on a person as they age and reach the period of senescence. But it is not only humans and our medical community that are attempting to arrest this mechanism, the cells themselves also have several ways to extend our lifespan beyond what they would normally be without them. An important part of this, and for the discovery of which the 2016 Nobel Prize in Medicine was given, is the system of autophagy.
Inherent Recycling
The two part process of autophagy involves taking useless components like misfolded proteins and worn out cellular organelles and recycling them by placing them into a specialized vesicle bubble named the autophagosome. This bubble then merges with a nearby lysosome in order for the latter’s degradative enzymes to break down those components into their individual molecular pieces for use in new parts of the cell.
It is the failure of this system to work properly that makes up many neurodegenerative diseases, like Alzheimer’s, where misfolded proteins build up in the cell and eventually lead to mass cell death. While research is being conducted in order to prevent these inaccurate proteins and other parts from being made in the first place, experiments involving autophagy are hoping to be able to break down these clogged up particles after that point. In short, it might be possible to help stop such diseases after their onset, rather than merely preventing them for others in the future.
A Complicated Pattern
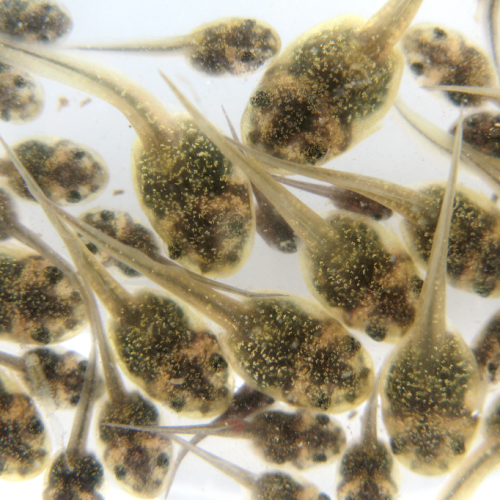
Past studies have shown that a protein called transcription factor EB (or TFEB) appears to be involved in the regulation and enhanced expression of genes connected to autophagy and the production of lysosomes. Researchers at Brown University found that there is an ortholog protein to TFEB that exists in the model organism Caenorhabditis elegans where it is called HLH-30. Its purpose appears to be multi-fold and beyond just autophagy and life extension, but also responses to starvation, heat shock, and bacterial infection.
However, for the autophagy process to be activated, the transcription factor proteins need to be localized in the nucleus to directly affect gene expression. That in turn is controlled by another highly conserved regulator called mTOR. It works to prevent that localization from naturally happening, so it is only when mTOR is inhibited that HLH-30 can reach the nucleus and begin autophagy production.
Unfortunately, similar past studies have shown that inhibition of mTOR causes a number of nasty side effects on the cell that would preferably be prevented if possible. So, scientists in the field of autophagy research have been looking for other activator systems that can work without mTOR needing to be involved at all. Those same Brown University researchers decided to run their own search and came across another conserved gene named Exportin-1 (or XPO1 for short) that strongly exports any proteins containing high leucine levels.
Lifespan Improvement
Their experiment with C. elegans was to see whether knocking out the function of XPO1 would in turn increase the activity of HLH-30 and cause autophagy to turn on. Simple enough and straightforward, though their initial search that found the gene was fairly long and arduous. They had to use an RNAi screen over the entire genome after fusing HLH-30 proteins to Green Fluorescent Protein (GFP) to see what genes were activated when the fusion protein was being exported away from the nucleus, something the scientists didn’t want to happen.
Upon silencing of the gene, they found that HLH-30 protein localization was heightened significantly. An autophagy reporter was used to measure the subsequent autophagosome and lysosome activity. A transgenic nematode with a condition similar to Alzheimer’s was used in order to test the effectiveness of knocking out XPO1 as a possible treatment. They found that the paralysis symptoms of the disorder were reduced and that, for an additional Huntington’s model, the amount of deformed aggregate proteins decreased substantially.
Furthermore, the lifespans of the nematodes with the knocked out gene increased on average from 15 to 45%. The difference in amounts appeared to relate to whether the gene was fully knocked out or just inhibited through the use of particular pharmacological compounds. Since the gene and its exportation function is still important for the cell, it appears to work better if its activity is just lowered, but not ceased completely. Tests with inhibitors like the compound KPT-330 proved to be strong enough to allow HLH-30 and other important autophagic proteins to localize to the nucleus, while still having XPO1 work to remove other proteins from the region that should be moved elsewhere.
The Future of Human Life
A final part of the experiment wanted to confirm that these effects could also be seen in human cells and with the original TFEB protein. Thus, HeLa cells were used along with a TFEB-GFP fusion proteins and selective inhibitor compounds of nuclear exportation. As expected, XPO1 was inhibited and this allowed TFEB to enter the nucleus, begin autophagy, and presumably improve organismal lifespan and neurodegenerative disease resistance, if it wasn’t for the fact that these were just a culture of cells.
The researchers hope that these similar inhibitory medicines can be used in a more directed fashion in the future to even better treat neurodegenerative disorders and they might even see a use in life-extension research and applications if similar lifespan improvements are seen in humans proper through XPO1 inhibition. But we’re a long ways off from human trials for such a thing. It will be something to look forward to.
Photo CCs: Caenorhabditis elegans DAPI from Wikimedia Commons