The research into new forms of CRISPR seems never-ending. It is an ongoing goal of scientists around the world to expand scientific knowledge on different kinds of CRISPR and also creating newfound capabilities for the existing varieties. Since the greater the flexibility of the tools available to science, the more treatments and medicines that can be devised from using those tools.
One of the topics that was unfortunately not covered by Bioscription in the past when it was reported on or in the long-form primer article on CRISPR was an expansion to the Cas9 system that allowed it to be used on RNA as well as DNA. This specialized form of CRISPR-Cas9 is in some cases preferred to the only other RNA-based system available currently, Cas13 (formerly C2c2). You, dear reader, can find out more about that particular system here.
Due to the greater all-around understanding of Cas9, it is often easier to work with due to past experience by researchers. But let’s discuss a bit on what exactly those scientists did last year to change Cas9 into its novel form.
A Better Description of PAM
This change relies on the accompaniment to the Cas9 protein, the short guide RNA sequence (sgRNA) that directs it toward its target and notes in its coding the correct sequence to cut. This sequence is made up of two parts, the complementary version of DNA from the original invading virus it was copied from and what is called the protospacer adjacent motif (PAM) sequence. The latter is one of the most important parts of the entire system.
To explain it in a better way than has been done here in the past, let’s go further back. The CRISPR system as a whole is a bacterial defense mechanism that looks for and destroys invading viral DNA strands. However, for it to recognize such attacks, the bacteria must have first been assaulted by a virus and defeated it. Upon doing so, it takes a part of the viral DNA and saves it as a protospacer in the CRISPR locus area, a sort of memory or reference bank for the future.
The PAM sequence revolves around all of this. Each motif is unique depending on the CRISPR system and the bacteria it’s in. For the original Cas9 system found in S. pyogenes, the PAM sequence is NGG, where N is any nucleotide (A,T,C, or G) and GG is obviously two Guanine nucleotide bases in DNA.
A Safety Mechanism
What the Cas9 system for this specific bacteria does is, when it is choosing what part of the defeated virus’ genome to save, it looks for an NGG sequence and copies part of the genetic code directly in front of it, but not the NGG itself. It is basically as if the PAM sequence is the parameters in a internet search that decides what gets pulled up and used in said search. Why do all of this? What’s the point of only copying sequences ahead of a PAM sequence?
The purpose is for the bacteria to protect itself. Since the Cas9 and CRISPR system in general is not very good at discriminative between friend and foe. If all that mattered was recognizing the sequences that the guide RNA points to, then that might lead the Cas9 protein to start cutting the bacteria genome at the place where the viral sequence was inserted to save. Which likely wouldn’t end well.
Now, Cas9 will only cut a DNA strand if the complementary guide RNA can bind to it and there is a PAM sequence after. Since the host bacteria purposefully did not include the PAM sequence when it copied the viral DNA, only an invading virus should have it. So, the safety mechanism protects the bacteria from itself.
Restructuring PAM
With the PAM sequence better explained, let’s get back to last year and what the researchers accomplished then. First off, an RNA-focused CRISPR system, like Cas13 is, doesn’t require a PAM sequence. Since there isn’t a risk of it attacking its own genome, as it only targets RNA and not DNA. For the scientists working with Cas9, this posed a problem, since they wanted it to be able to cut RNA, but it was specifically evolved to focus on DNA and wouldn’t work without a PAM-like end target.
Past research in 2014 had been able to at least slightly get Cas9 to work on RNA by combining the PAM sequence for it with an oligonucleotide, which created what is called a PAMmer.Thanks to the nucleotide, it is able to hybridize with the target RNA and thus let Cas9 recognize it as the end sequence and cut the RNA. But this was only ever tried in vitro in a test tube and not in an actual bacterial or living organism environment.
For the researchers last year, to lead the way toward programmable RNA targeting by Cas9, they modified the PAMmer structure to make it more stable. Then they modified various parts of it as guide RNA and tried it in living cells. They were successful, opening the way toward an RNA-targeting Cas9 that could be used to modify cellular transcription actively.
Altering RNA
Which leads us to today, finally. Researchers at UC San Diego have used the RNA-focused Cas9 they developed last year, which they have dubbed CRISPR-RCas9, to target microsatellite repeat expansions.
These are repeated sequences in the genome that are prone to a particular kind of duplication mutation that results in the repeats getting longer in subsequent human generations. When translated into proteins, they go haywire and make it impossible for the protein to fold properly into its active state. These broken proteins then build up in the cell and cause other problems.
This means that an otherwise healthy gene with no mutations directly in it cannot be properly transcribed because of the repeats that follow after it. These defects are commonly found on genes coding for neurologically-active proteins and their, more or less, inactivation by the repeats causes many neurological disorders. This includes Huntington’s disease, myotonic dystrophy, and a particular form of amyotrophic lateral sclerosis (ALS), among others.
To End Neurological Diseases
With RCas9, the researchers were able to target these repetitive sequence RNAs and destroy them before they were translated into proteins. This can include cutting away the broken repetitive segments. At least on a cellular level, this appears to result in a full recovery of symptoms from the diseases, with there no longer being a buildup of toxic proteins in the cellular matrix.
Thanks to this success, they can now move forward toward animal model testing and eventual human trials that may finally cure some of the more pernicious of the neurological diseases. And do so on a scale that doesn’t change or alter DNA in any way, but targets the RNA expression of those genes.
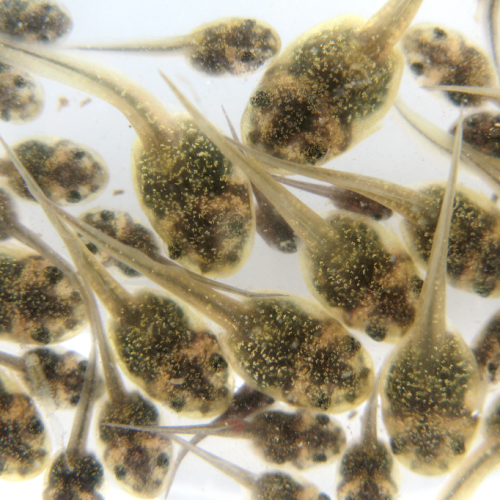
Photo CCs: Neuron-matrix from Wikimedia Commons