As food and agriculture have expanded through global cooperation and innovation, this has coincided with a greater ease in developing high-selling products such as sugar. The downside of this new capacity is that many food products have begun to use at least a small amount of sugar to improve taste of those same foods and increase sales. However, this has also resulted in not just higher sugar intake, but higher calorie intake on average in total in developed countries. This has, predictably, caused conditions like obesity to skyrocket and become far more common than they were previously. Coinciding with this has been several comorbidities like heart disease and diabetes.
How Obesity Works
Therefore, heavy amounts of research have been put into studying how these conditions develop and what changes they make to cellular production, in order to possibly find ways to alter human metabolisms to more easily prevent the disorders. What is already know is that there are two primary methods for compiling fat tissue and they make up the two forms that obesity can take.
The first is the process of hyperplasia, where new fat cells are made by differentiation of the old ones, thus creating larger total fat deposits. And the second way is hypertrophy, where the existing fat cells, called adipocytes, expand their storage to be able to hold even more lipids. The latter is bad due to excess lipids being stored elsewhere in the body, leading to lipotoxicity, which itself causes insulin resistance, cell death, and other conditions.
All of this contributes to what is referred to as the adipose tissue expandability hypothesis. This hypothesis is based on the idea of how the process of fat deposition works, where energy is stored in fat stores and, once those are full, the adipocytes begin to grow to store more lipids, along with storing lipids in other regions of the body. Lastly, once the fat cells have become as large as possible, pre-adipocytes are then used to split and produce new cells. This forms the presumed final limit on what expansion is allowed.
Creating Fat Cells
The mechanisms of differentiation of fat cells from their stem cell state to their final adipocyte form have yet to be fully understood. Therefore, scientists at American University decided to use adipose-derived stem cells (ASCs) in order to better probe how the differentiation steps take place. These stem cells can be easily obtained using liposuction techniques and they readily form into not just adipocytes, but also chondrocytes (cartilage cells) and osteocytes (bone cells) if they are exposed to a specially formulated hormone solution.
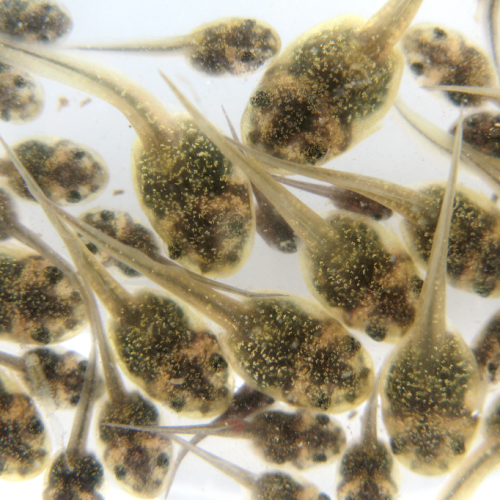
And this is precisely what they did, setting up three different experimental groups to try and make all three types of cells. The transformation into differentiated cells was conducted over a period of two to three weeks. Surprisingly, the adipocyte differentiation appeared to result in two distinct populations, the normal and expected ones containing lipid stores and an unusual additional group lacking those same lipids and instead resembling more their original stem cell form. This unexpected group was found to replicate quite readily, unlike true adipocytes, raising further questions.
After collecting RNA samples and running a Principal Component Analysis on the gene expression in this unknown group of cells as compared to the original stem cells and the properly differentiated adipocytes, the researchers were able to make a spectrum of the path to their final form. These lipid (-) cells appeared to be somewhere in the middle, though not that far off from the adipocyte end of things. This allowed them to conclude that these weren’t normal stem cells, but were in fact at least partially differentiated. With some further data crunching, they were able to come up with the 39 genes that matched with adipocytes, giving even further insights into essential gene functions transitioning from the intermediary lipid (-) state to the end adipocyte state.
Unexplained Cells Explained
These genes also showed how the lipid (-) cells were resisting the change to full differentiation that the hormone media was pushing on them. Interestingly, they were still displaying two of the three characteristics that have been determined to identify stem cells over other cell types. Nearly the full three even. They are able to adhere to plastic, they still have the capability to differentiate into any of the three cell types, and they have two of the three surface markers that showcase them as stem cells. Yet, at the same time, they have far closer gene expression to adipocytes than to stem cells.
So these unique cells are close to being adipocytes, but fulfill all the criteria for being multipotent. By almost accident, the researchers were able to find a previously not known stem cell-like multipotent fate that doesn’t require the involvement of other cells types and instead is based around the intrinsic fate determination in vitro, as they were obtained from fat deposits originally. Cells with these characteristics are not entirely unheard of, as similar ones have been found with skin cells, gut cells, blood cells, and neurons, but this is indeed the first time with fat cells.
They hypothesize that this group of lipid (-) cells may be a certain mechanism used by the human body to keep adipose expandability available. The mechanism controlling the inherent limit to differentiating new adipose cells had been unclear, but it is highly likely this group is responsible for that factor.
Preventing Lipotoxicity
The scientists propose that when all of these lipid (-) cells have been depleted through differentiation, the ability for more fat expansion is lost or curtailed, leading directly to hypertrophic obesity. That, in turn, leads to lipotoxicity. On the other hand, if too many lipid (-) cells are made, that could also lead to the same due to how they are slow to differentiate and may not be able to make enough adipocytes in time to avoid the result of obesity.
With this study, the American University researchers have not only found the first case of cellular multipotency in fat cells, they have also discovered a key component to obesity, BMI, weight gain, and all of the connected diseases that afflict those suffering from the condition. More research, they hope, will further elucidate this involvement and offer solutions or at least options to prevent or slow down the onset of obesity.
Photo CCs: Adipogénesis from Wikimedia Commons