The field of study involving infectious diseases is complex. There’s no reason to downplay that fact. There are a huge amount of variables to consider when dealing with disease outbreaks and differences between viral, bacterial, parasitic, and other disease-causing vectors are immense. But at the same time, one of the goals of epidemiology and immunology is to be able to express that complexity in a simpler way, to at least be able to get across the gist of the relevant factors that both scientists and the general public need to care about.
It’s because of that that complicated topics such as just how virulent a pathogen is or how infectious it may be from one strain to the next are often depicted in specific numbers that may simplify the underlying math, but that at least convey some understanding of how dangerous one disease is to another. There are plenty of explanations of these sorts of data, both written and visual, that do an incredible job at informing those who may not have the scientific background to be intimately familiar with such topics. I make no assumptions that this article will prove to be better than any of those other attempts, knowing that the opposite is likely true. But if even a single person can come away from reading this article more personally informed and knowledgeable about the subject, then that will be a goal accomplished.
If you haven’t guessed now from the title or even the vague allusions in the paragraphs above, this article is about the coronavirus, SARS-CoV-2. Though we will also delve into more general aspects of how virology research is conducted, what the common terminology means when discussing viral disease outbreaks, and what specifically are the characteristics of the Covid pandemic in relation to other diseases. And we’re going to start very simply with the R0 number (verbally spoken as R naught), as this is one of the fundamental aspects to wrapping your mind around the spread of a disease. You may already have a good grasp of how it works and have seen the many great graphical representations of it, but for everyone else, let’s talk about it.
The R0 of a Disease
The R0 is known in full as the “basic reproduction number” and can be used to determine just how contagious a pathogen is. This relates to infectivity and pathogenicity, which is covered in the next section, but here’s the direct explanation. This reproduction number is a reflection of the number of people that a single infected person will go on to infect. While usually represented as just a single number, sometimes with a decimal point, there’s a lot more going on behind the scenes to determine it and it is, in reality, not static. Not only will different variants likely have a change in the number, it can also vary depending on environmental conditions and our very own actions (Delamater 2019).
Since the entire point of safety protocols and measures against a disease during a pandemic is to reduce that R0 number below 1, so that less people will be infected from each infected person with each subsequent generation of it spreading. It is reducing the number below 1 that successfully manages to end an outbreak. We can reduce it by reducing exposure to infected individuals and also by being vaccinated so we produce less of the pathogen if infected and spread it far less. This is, of course, more difficult the higher the initial R0 is for a specific disease, as you have to put more effort and be even more vigilant the more infectious a specific disease is.
It’s because of these variables and many others that determining an R0 can be rough, particularly in trying to reduce it down to a single number. Different areas of the world may conceivably have different R0s to deal with even if the same strain and variant is in both locations. Varying levels of hygiene, the existence of fresh water and working sewage systems, and just the availability of basic medicines can all impact the resulting infectivity levels. These can even vary on a person to person basis, since as pointed out before, it is your own safety precautions that determine how much you reduce the R0 risk that you are exposed to and expose others around you to. And contact tracing of individuals and what other infected people they have been exposed to is a primary part of figuring out the R0 of a disease as it is (Breban, Vardavas, and Blower 2007). So while the number is informative, particularly as a comparison to other diseases, it still comes down to the fact that you as a person determine the real R0 and your own risk of exposure.
But there are also factors related to the pathogens themselves and how they mutate that can change the R0, so let’s go over those as well.
Virulence, Transmission, and Pathogenicity
One of the problems that scientists face when trying to describe terms like how virulent a pathogen is is that there are major disagreements between different fields of biology and are often dependent on what kind of pathogen is being investigated, such as fungal, bacterial, or viral, but then even more differences dependent on if the pathogen is attacking humans (making it medicine research), other animals (making it ecology research), or plants (making it a mix between ecology and agricultural research depending on the plant in question). And don’t forget insects or the microbes in the soil or any number of other topics. There is no one agreed upon definition for these terms and there have been arguments about them going on nearly a century now.
The general understanding of the term virulence is fairly straightforward, it means just how severe and harmful a disease is. The more virulent, the more harm it will cause. Which is likely why the word itself has also come to mean (or perhaps meant before the scientific usage) hostility and anger, usually in regards to using harmful language. And in most medicine-focused research, that’s precisely how it is used with viruses and bacteria. And it also forms the basis of one of the most common statements about diseases, that there is a tradeoff between virulence and transmission. The greater the ability of a pathogen to infect others (which can be represented by the R0 we just discussed), the less virulent it is expected to be. Since if a disease is too harmful and especially if it is too lethal too quickly, that will reduce the ability for it to spread fast enough to keep an outbreak going (Thomas and Elkinton 2004).
Though, as discussed in the Covid section below, we have found that said commonplace belief in medical science isn’t always the case if certain traits are present in the disease. But, getting back to virulence, a different way it is understood is directly tied to how lethal it is, with toxicology researchers using virulence to refer to another term, the Lethal Dose 50% (LD50). This is the dose required of a toxic chemical to kill 50% of the test organism exposed to it, such as mice or insects. Transmission in this case is assumed to be 100%, because virulence only applies to the impact it has on the organism that is already infected or exposed (Day 2002). A very different and opposing look at the term in a different field of science, though one that doesn’t have much to do with Covid. Since this is indeed a medical matter.
Before we move on, we’ll have a brief interlude with another term: pathogenicity. This one is even more ill-defined than virulence and has far more conflicting accounts. In many cases it is simply used as a synonym for virulence and no more thought is put into it. Other scientific fields use it as a term that is much closer to transmission, and thus the R0, than how harmful a disease is. These other ways define it more as how “aggressive” a disease is and how well it can infect its hosts, with a focus not being on just infections, but also the way that a pathogen develops new ways of infecting and getting around defenses. Pathogenicity is used almost as a measure of how active and alive the pathogen is, along with how quickly it develops new measures to harm its target (Shaner et al. 1992). This makes it a word that is distinctive from the simple R0 number and provides more focus on dealing with the disease as an entity itself and how the disease develops after infection.
Whether that is more philosophical than useful is for you to decide. But hopefully this gives a better understanding of these terms and how they are used in science and medical settings. Now, let’s move on to the star of the show, the actual pathogen that is the point of this article.
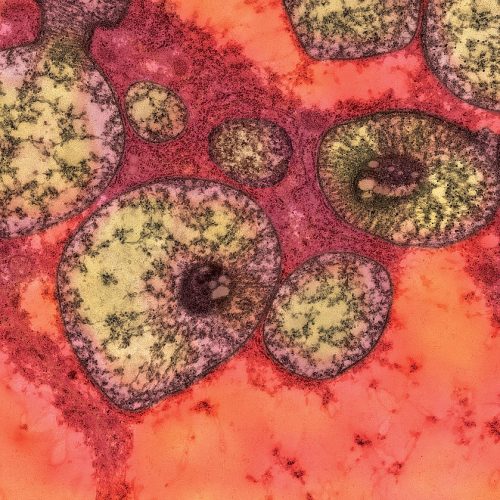
Virulence Characteristics of SARS-CoV-2
Let’s start at the beginning with what we started with in this very article, the R0. There have been multiple variants of concern as the Covid pandemic has spread and we’ll go over variants next, but we should start with the original strain before any variants occurred. That strain is also referred to as the “ancestral” strain and, as its name suggests, is in the same family group as the SARS outbreak of 2003 and ongoing MERS outbreaks since 2012 (Viceconte and Petrosillo 2020). Like those, it begins as a respiratory illness, though we have found that it then progresses to a vascular disease spreading throughout the bloodstream and causing damage to external (epithelial) cells on organs. We continue to find new problematic facets to what it is capable of every day and it is clear that there are multiple far reaching impacts of infection that can reduce quality of life even if it proves to not be fatal.
Because of those varying factors we discussed that can alter the R0, the range of possible numbers for Covid, even with the original strain, was considerably wide even after reported by the WHO, differing from 1.4 to 2.5. At the beginning, this seemed manageable and it was expected by the medical and scientific communities that we would be able to deal with and contain the pandemic before it even got going. After all, it’s no measles, with an even more extreme R0 range of 12 to 18 people being infected per single infected person (Guerra et al. 2017). An outbreak of a disease with Covid’s characteristics and that R0 would be a catastrophe of almost immeasurable proportions, especially since a higher R0 also correlates to how difficult it is for someone’s immune system to fight off infections.
Some locations around the world had results indicating a much higher R0 for Covid, which may relate to higher exposure risk and greater population density, further showcasing how other variables can change the number in question. And different methods of modeling the spread of the disease and the data available for how it spread through the contact of people can result in major discrepancies. But we can still control for these and compare Covid at least with other diseases, including its own variants, to determine which have higher transmission.
A major issue with Covid that increases its potential for mutation and variation is the fact that the family that makes up coronaviruses have a massive amount of potential host species. As we’ve seen with Covid itself, many, many mammals can be infected and then pass on that infection to not only others of their species, but also back to humans. This sort of infection is called zoonotic transfer and terrifies every scientist that studies human diseases, as it is one of the sources of large scale mutations and the creation of worse versions of the pathogens we already have to deal with (Sarkar and Guha 2020). Particularly if infection occurs in the same cell with different viruses, opening the possibility for recombination to occur between them, where they would essentially share traits. This could result in nothing or even harm both of the viruses, but there is the potential for the subsequent generations to be even worse than they were originally.
Variants and How They Get Worse
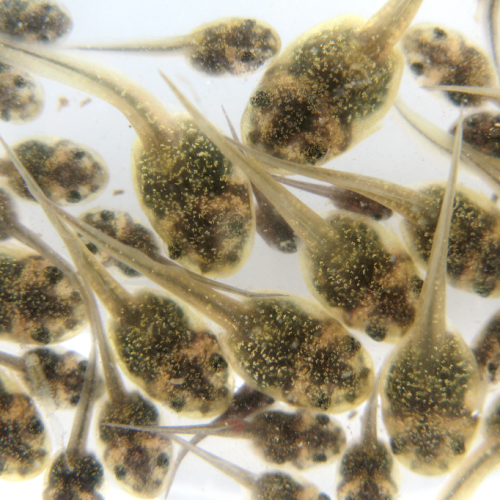
As I’m sure you’d heard plenty over the past two years, we’ve got some variants going around. Quite a lot of them, in fact. And likely much more than you’ve heard of, as at least a dozen or more variants never gained any traction and faded away, never reaching levels where they were included in official lists of concern by the WHO or other organizations. But how do these variants emerge in the first place and what do we even mean by the word variant?
We mentioned before that the original or ancestral strain refers to the first observed strain of a virus. After that point, any new version of that strain that has a difference in its DNA, its genetic code, we refer to as a variant. When it comes to those diseases that are medically relevant, we primarily only classify variants that have differences in their DNA that relate to their ability to infect their host or replicate themselves, as those are the only traits relevant to consider from a medical standpoint. Any mutations or changes to the genome of a virus in another part of its sequence remains largely irrelevant if it doesn’t have an impact on the virus’ ability to go through its life cycle.
The reason these mutations happen is because when a virus infects a cell, it begins using the cell’s machinery to build more of itself so that these new viruses can go out and infect more cells. But the copying machinery isn’t perfect. When making duplicates of the virus’ DNA, there are occasionally mistakes, what we call mutations. Depending on the virus, this can happen more or less often. Part of this depends on if the virus has a genome made of DNA like ours, so a double-stranded genome, or if it has a genome made of RNA, which is single-stranded in most cases (there are exceptions with viruses, such as having single-stranded DNA and double-stranded RNA, but we won’t get in that here).
This is because DNA and RNA have different replication machinery in the cell and RNA is far more prone to mutational mistakes being made. That’s also the secret behind influenza, which is also an RNA virus and it mutates incredibly fast, making the development of vaccines tricky and an ever ongoing process. Luckily, coronaviruses are not as bad as that, as they have an extra piece in their genome that allows for a form of proofreading and error correction to occur on their replicated genome, greatly lowering the amount of mutations that happen. This makes Covid much more stable and, if you can believe it, makes far fewer variants occur in the same time period. So all the variants we’ve seen are minimal to what they could have been otherwise (McNeil 2021).
In Brief: Variants We Know
There’s a lot to cover in this particular subsection and massive lists of variants that will not be discussed here. But we can quickly go over the variants we know about and how they’ve changed in regards to R0 and virulence in comparison to the ancestral strain. The variants that reach levels where a significant amount of transmission are being seen in the general community are usually upgraded to being called variants of concern (VOC) and this is the point where they get an official name designation beyond their original serial number (Kannan, Ali, and Sheeza 2021).
As an example, the first variant to emerge to popularity was dubbed the Alpha variant (previously referred to as the B.1.1.7 variant) with its official reporting happening in December of 2020 in the United Kingdom, though low levels of it had been circulating for several months prior. It was a bit of a doozy as well, as it had significantly higher transmission numbers, resulting in a new R0 that was 50% greater than what was reported for the ancestral strain (van Oosterhout 2021).
Then came the Beta variant in South Africa, which had actually been known about for months earlier than the Alpha variant, since May of 2020, but never increased in number of infections and so was never officially named as a VOC until much later. While lacking the transmissibility of Alpha, the Beta variant had changes to the receptor responsible for invading a cell, known as the spike protein. This raised concerns that it would be better able to evade detection by the immune system even after being vaccinated thanks to it no longer perfectly matching the spike protein the immune system was primed to detect. But the lowered transmission meant it never was able to spread as quickly or as well as the Alpha variant and later variants, making it not a major problem in the long run. For now, at least (Duong 2021).
After that came the Gamma variant in Brazil, first noted in November of 2020 and becoming more dominant in the region as 2021 progressed. This variant seemed like almost a combination of the previous two, having mutations that both increased transmission by nearly the same amount over the ancestral strain as Alpha and changes to the spike protein that slightly reduced immune system responses like Beta. While Gamma managed to become dominant for a while in Brazil and South America, it eventually was found to not be able to compete in the long run and became less consequential (Duong 2021).
Lastly, we have the very well known and famous Delta variant. This was found in India in October of 2020 and suddenly surged into prevalence in the middle of 2021, showcasing that with the lack of vaccinations worldwide, transmission was the major factor for success and not being able to get around vaccines that not everyone was taking as it was. Delta is over and again worse than the others, presenting a 60% increase in infectivity over the Alpha variant itself. In that regard, it’s R0 was calculated to be in a massive range, 3 in some places and 8 in others, with an average of 5 or more being most common. Compared to the ancestral strain barely reaching an R0 of 2 in most cases, the Delta variant was able to spread at an incredibly fast rate. This was combined with what we are still learning about the variant, such as an increased virulence and thus harmful outcomes and potentially a greater capability to evade the immune system and cause breakthrough infections in the vaccinated (though still at a far lower rate than those without the vaccine thanks to the body’s immune system being able to fight back faster and stronger with vaccine memory foreknowledge) (Liu and Rocklöv 2021).
Additional Concerns
So, we’ve covered a lot thus far and hopefully provided a ton of information about how virus research works, how outbreaks and epidemics are measured, and what we know about SARS-CoV-2 thus far. But even with all of that knowledge now obtained, do note that Covid is far from our only concern and instead should serve as a warning for the future. Because it’s unlikely that this will be the only pandemic we will have to deal with. And while other disease outbreaks may have a smaller result on their own, they also shouldn’t be underestimated. You can never tell when a new strain of a pathogen or a variant of an existing strain will emerge and prove troublesome.
With that in mind, let’s briefly go over some other concerns that have cropped up in the past two years and the ongoing diseases we should keep an eye on. One is an old and familiar favorite: measles. This virus has been a constant hazard even in modern life and new outbreaks are always prone to occur if vaccination efforts dip by even a few percentage points, which has been observed particularly in the past few years. Because measles has an R0 of a much greater amount, as previously noted, it spreads through populations much quicker and it has taken advantage of the past two years of the pandemic to do just that. Especially in the developing world and in low-income regions (Rana et al. 2021).
It may be that due to efforts being focused on dealing with Covid, measles vaccination campaigns have been forced to fall to the wayside, allowing for new outbreaks in Pakistan, India, and throughout Africa and South and Central America. The number of deaths seen since 2016 aren’t minimal either, reaching hundreds of thousands, and a significant amount of those are among children. Particularly those young enough to still have developing immune systems and not having proper defenses to fight off a measles infection. Hopefully we will be able to balance all of our disease fighting efforts in the future so we can continue bringing the siege against measles while also simultaneously dealing with any future Covid concerns and other diseases.
Speaking of other diseases constantly lurking on the periphery, there’s chikungunya to worry about, another of the colorfully named pathogens brought to us thanks to the efforts of the invasive Aedes aegypti mosquito. If you couldn’t guess, there’s a lot of horrifying things we have A. aegypti to thank for bringing back to cause new outbreaks again and again. In the case of this viral pathogen, lethal outcomes are rarely the main concern, but there are plenty of significant health problems and life-long symptoms that one may have to contend with if they contract it and there is no real treatment for it at the moment that has any sort of efficacy or widespread distribution (ECDC 2021).
One of the problems specific to chikungunya due to its mosquito vector is that it can pop up in new outbreaks practically anywhere with a warm climate, with cases being counted in 2021 across the Americas, the Middle East, and southeast Asia. This makes it difficult to contain, though efforts to do so to the mosquito in general are ongoing, since it is the vector for numerous diseases and eradicating it would be beneficial to the surrounding environment as well, since it is non-native in most of its current range. As temperatures continue to rise thanks to climate change, the potential range the mosquito can live and reproduce in will similarly expand as well, creating an ongoing and ever worsening problem for North America and Europe in particular.
And while we’re on the topic of diseases Aedes spreads, that also include dengue fever that has seen a massive outbreak worldwide starting in 2019 and ongoing today with millions of cases. South America, southeast Asia, and India have been among the hardest hit, with the new outbreak in India as of the past two months being the largest recorded in several years (Sharma 2021). Deaths have increased as well, specifically among children, and ever more expanded efforts to destroy mosquito breeding groups are being conducted in response.
In Conclusion
So, as you can see, we have epidemics being fought on multiple fronts and we shouldn’t ignore any of them, lest they contribute to a new pandemic we have to concern ourselves with. But we have the technology and the means to combat all of them, as we have been doing. It just requires concerted effort and global cooperation to do so, as lacking as that might have been in the past two years. Hopefully new scientific research and medicines will allow us to deal with these pathogens and more in both the short and long term and reduce the potential for more deaths and health impacts at the same time.
To accomplish that, we all have to stay informed and educated on how diseases work, what we are doing to fight them, and what contributions each and every one of us can make every day to keep ourselves and others safe. Since when it comes to contagious diseases, protecting yourself is the same as protecting others and we all contribute to the well-being of the community around us.
References
- Breban, R., Vardavas, R. & Blower, S. Theory versus data: How to calculate R0? PLoS ONE 2, (2007).
- Chikungunya worldwide overview. European Centre for Disease Prevention and Control (2021). Available at: https://www.ecdc.europa.eu/en/chikungunya-monthly
- Day, T. On the evolution of virulence and the relationship between various measures of mortality. Proceedings of the Royal Society of London. Series B: Biological Sciences 269, 1317–1323 (2002).
- Delamater, P. L., Street, E. J., Leslie, T. F., Yang, Y. T. & Jacobsen, K. H. Complexity of the basic reproduction number (R0). Emerging Infectious Diseases 25, 1–4 (2019).
- Duong, D. Alpha, Beta, Delta, Gamma: What’s important to know about SARS-CoV-2 variants of concern? Canadian Medical Association Journal 193, (2021).
- Guerra, F. M. et al. The basic reproduction number (R0) of measles: A systematic review. The Lancet Infectious Diseases 17, (2017).
- Kannan, S., Ali, P. & Sheeza, A. Evolving biothreat of variant SARS-CoV-2 – molecular properties, virulence and epidemiology. European Review for Medical and Pharmacological Sciences 25, 4405–4412 (2021).
- Liu, Y. & Rocklöv, J. The reproductive number of the delta variant of SARS-COV-2 is far higher compared to the ancestral SARS-COV-2 virus. Journal of Travel Medicine (2021).
- McNeil, T. How viruses mutate and create new variants. Tufts Now (2021). Available at: https://now.tufts.edu/articles/how-viruses-mutate-and-create-new-variants
- Rana, M. S. et al. Emergence of measles during the COVID-19 Pandemic Threatens Pakistan’s children and the wider region. Nature Medicine 27, 1127–1128 (2021).
- Sarkar, J. & Guha, R. Infectivity, virulence, pathogenicity, host-pathogen interactions of sars and sars-cov-2 in experimental animals: A systematic review. Veterinary Research Communications 44, 101–110 (2020).
- Shaner, G., Stromberg, E. L., Lacy, G. H., Barker, K. R. & Pirone, T. P. Nomenclature and concepts of pathogenicity and virulence. Annual Review of Phytopathology 30, 47–66 (1992).
- Sharma, S. Dengue suspected of killing dozens as Indian state suffers worst outbreak in years. Reuters (2021).
- Thomas, S. R. & Elkinton, J. S. Pathogenicity and virulence. Journal of Invertebrate Pathology 85, 146–151 (2004).
- van Oosterhout, C., Hall, N., Ly, H. & Tyler, K. M. Covid-19 evolution during the pandemic – implications of new SARS-COV-2 variants on disease control and public health policies. Virulence 12, 507–508 (2021).
- Viceconte, G. & Petrosillo, N. COVID-19 R0: Magic number or conundrum? Infectious Disease Reports 12, (2020).
Photo CCs: SARS-CoV-2 illustration (18) from Wikimedia Commons