Being able to edit the genome of living people has been a long sought after goal of medical research in order to cure any number of genetic disorders. Most such editing research is only able to affect such changes either on a generational level by changing eggs in vivo or in a localized area of specific cell types in a person’s body. This is even more limited by the fact that the vast majority of this field of study and its successes have only been in altering genes in the nucleus of cells. The mitochondrion is a whole other story, but a very important one. As you know with how much of a “powerhouse” the mitochondria are, there are a vast quantity of important genes and regulatory pathways that are controlled through the mitochondrial genome. To put it simply, you would not be alive without them.
Dealing With Mitochondrial Disorders
It is also because of this that mutational effort in mitochondrial genes are so debilitating and cause disorders that drastically shorten someone’s potential lifespan. This is especially so for mammals, who have much less wiggle room for where mutations will land than other species, such as plants do, in their mitochondrial genomes. It is also for this reason that mitochondrial disorders are among the most common that are passed on through families, affecting about 23 out of every 100,000 people. So being able to modify the genome in your mitochondria is an important avenue of research in medicine. And one that is, at this point, more fraught with difficulties than nuclear genome research.
Because one does not simply modify the mitochondrial genome. Transporting the desired editing machinery, such as a CRISPR complex, into the mitochondria is troublesome to say the least and, to this point, largely only small restriction enzymes and some nucleases targeted to the mitochondria to cause targeted damage to problem genes has been the extent of our capabilities. The ability to freely enter and manipulate the mitochondrial genome is the holy grail of biological research both for plants and animal scientists. What the aforementioned products do allow us to do is affect the heteroplasmy of the mitochondrial makeup.
Reversing The Heteroplasmy
To explain this term, you first must be informed that your cells don’t just have a single mitochondrion apiece, despite what textbook diagrams might imply. That scenario is only the case for single celled organisms, since their energy producing requirements are so much lower, and even then it isn’t true for all of them. Your human cells, meanwhile, have hundreds, if not thousands of mitochondria per cell. With the number varying depending on the type of cell and what its function is in the body. And they all have their own genomes that don’t necessarily have the exact same gene distribution. It is that difference in distribution of versions of the same gene that is referred to as heteroplasmy, the existence of variant copies of the same gene within a cell.
This is highly relevant when discussing mitochondrial disorders, as they often only become a biological health hazard once the defective gene reaches over 50% heteroplasmy as compared to copies of the working gene. Of course, not all mitochondrial disorders are heteroplasmic, some have 100% defective gene copies, but we’re not focusing on those today. For all the rest, the ability to take out and replace the defective copies with working ones just enough to change that ratio is often good enough to effectively cure whatever mitochondrial disorder is occurring. So it is not an all or nothing scenario, which is very helpful when it comes to medical options. A lot less work and the difficulty of even modifying the genome of mitochondria makes that biological truth a godsend.
Deamination To A Cure
So, as noted, we’ve long had some options for upsetting that heteroplasmic order in mitochondria by cutting out the bad copies with restriction enzymes and hoping for the good copies to be transcribed in their place. Of course, with restriction enzymes and nucleases, the level of control is sadly lacking in many situations, but the scientific community has managed over the past two decades. But what if we wanted to actively change the variant genes into new working variants and not just rely on fixes from copying off of working genes? That would be much more efficient and effective. Well, we now have a tool for that referred to as DddA-derived cytosine base editor (DdCBE). A long name, I know.
In short, it allows for deamination, removal of an amine group, from cytosine. Which, due to the structure of the nucleic acids that make up your genetic code, converts the cytosine to a uracil. Uracil is just the RNA form of thymine. The cell corrects this, since uracil doesn’t belong in DNA and we have molecular processes to identify these problem cases, and replaces the uracil with a thymine. And, thus, we have changed a C-G code to a T-A code, changing a letter in our DNA. That’s a simplified explanation for what the DdCBE tool does and we have bacteria to thank for it, as the tool comes from a modified bacterial toxin utilizing the TALENs gene editing system and which is already set up to target the mitochondrial genome. So it was almost perfect from the beginning for our purposes.
For Mice And Beyond
And now, with this tool, we can directly change the letter sequences in the mitochondrial genome. Only one specific type of change, sure, but that gives a massive amount of leeway and options for fixing defective genetic sequences. In the past year, this tool has already been shown to work on embryos of mice and zebrafish. But researchers at the University of Cambridge wanted to go farther, to test the tool in living adult mice and show that it can alter mitochondrial genes successfully in the current generation.
They started by confirming the ability for editing in cultured mice cells and to compare DdCBE tools with the most efficient design among different TALE nuclease options. With that decided, they then went on to using an adeno-associated virus (AAV) vector to carry the tool into the adult mice and the focus on editing specifically the mitochondria of heart cells in the mice. They started with just born mice pups and found an overall 20-30% rate of successful conversion from cytosine to thymine among the mitochondria in the cells at the targeted gene site. This percentage was then found to be significantly lower among the adult mice and the scientists hypothesized that the higher ratio of AAV vector to number of cells to modify in the small young mice as compared to the older ones may have increased the efficiency outcomes.
Either way, they were able to confirm that the DdCBE tool does work on living multi-cellular organisms and their mitochondrial genomes. Even if the efficiencies in adults isn’t as high as would be desired, that is something that can be worked on and does allow simply for multiple treatments to be done over time to gradually alter the ratio of heteroplasmy in the genomes for reversion of the non-functional copies of the problem genes. The potential for treating mitochondrial genetic disorders has been expanded by the research and has opened the door for future experiments and the development of real treatments. We’ll just have to wait and see how things go as this exciting new tool and field of medical research continues.
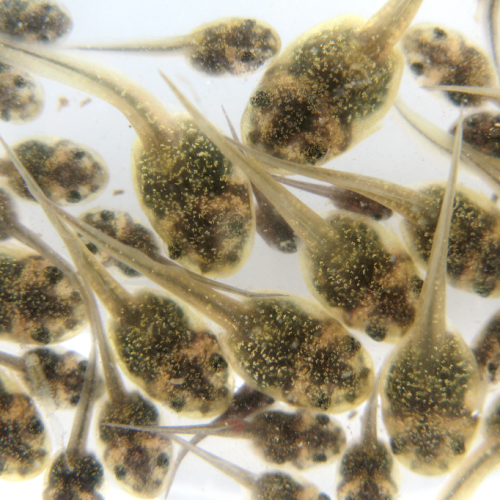
Photo CCs: Abnormal Mouse Mitochondria (44402464170).jpg from Wikimedia Commons