Personalized medicine has become radically different over the past decade. The speed and lowered cost of genome sequencing has made disease screening far more commonplace and as specific cell-based treatments have improved, some conditions that were once thought incurable are becoming very much not so. For immune system focuses, chimeric antigen receptor (CAR)—T cells have been an oft spoken of treatment method, especially in trying to deal with the hundreds of variants of cancer formation.
Inducible Genetics
Synthetic biology as a whole has seen a boom in genetic expression-based technologies. The therapies required to treat certain disorders require a controlled uptake of medicines and other compounds, which can be done through epigenetic manipulation. If you can control which genes are “turned on” and thus transcribed into RNA and proteins, then you can manage how a cell responds to its environment. For many of these switches controlling genes, scientists had to set them up to respond or be induced by certain molecules that are rare enough that they wouldn’t be accidentally activated.
The original sources of inducible control used in the medical field were antibiotics themselves, since a doctor had to prescribe them directly. But with issues like antibiotic resistance cropping up, alternatives were sought over the past several decades. Some found some favor, like vanillic acid or plant metabolites, but concerns of side effects remained even with these. Very recent studies have even been able to use temperature control or light control via lasers as an option. Though that tech is still too recent to say whether it would work in the long term.
So the search has continued. What medical professionals need is a substance that is inexpensive to obtain or produce, has no meaningful side effects, and is limited in occurrence in the world at large.
Caffeine-Powered Insulin
Researchers from Switzerland and France have now decided to tackle the topic with their own inducer, a quite obvious and apparent choice when you think about it: caffeine. Since caffeine isn’t all that toxic, especially at the low doses we use it at, it is easy to produce in mass quantities, and it isn’t normally found in foods and produce outside of caffeinated beverages and chocolate products. Therefore, caffeine-responsive gene switches were, to them, an easy choice, though their tests in yeast did have an additional complication for that species.
In order to properly activate the connected genes, the yeast needed to transform the caffeine into the compound theophylline. But it has low sensitivity for noticing physiologically relevant caffeine in its surroundings. So they went with a more complicated approach in mammalian cells.
The first step was to find an antibody that has a high affinity with caffeine, which they did discover and use in one named aCaffVHH. They then fused this antibody with several signaling receptors from different kinds of mammalian cells, creating a fully synthetic receptor system able to sense caffeine even at the small amounts ingested from a cup of coffee. This new system was termed C-STAR (caffeine-stimulated advanced regulators) and is able to stimulate insulin production genes in the presence of caffeine.
.
Testing C-STAR with petri dish embryonic kidney cells with diabetic genes and also two mouse models that have been designed with Type 2 diabetes, they were able to confirm its functionality with a variety of consumables, including coffee, tea, and energy drinks. It was a perfect match because insulin production is often needed after a meal and one could just consume such a drink with the meal to activate the system.
The appropriate activation of C-STAR was controlled by using a cell transmission method, which were microencapsulated and implanted into the mice. The regulators included transgenes in the cellular genome that would produce insulin upon startup of the receptors due to caffeine. The homeostasis balance of glucose was observed to remain much more level after insertion of the modified cells.
Genetic Switches To Control Disease
Future experiments will be required to put this system into human cells in particular rather than generic mammalian species, but its success should translate properly. In the future, perhaps even the near future, we may see treatments that involve the addition of these cells (in kidney cell or really any other form) to a person’s body in order to cure them of their diabetes by returning to them their ability to produce and regulate insulin.
Of course, this would still mean a lifestyle change, as they would personally be controlling when such production occurs, but in a manner that is far easier and better than having to use frequent injections for the same purpose. The researchers hope that they will be able to take advantage of natural cultural consumption trends so as to easily incorporate such things into the normal habits of diabetics that take the treatment. They also envision a world where multiple treatments for all kinds of similar diseases are seamlessly made a part of everyday life with little fuss or extra effort.
A world where no one has to be sick and where everyone can live their normal lives.
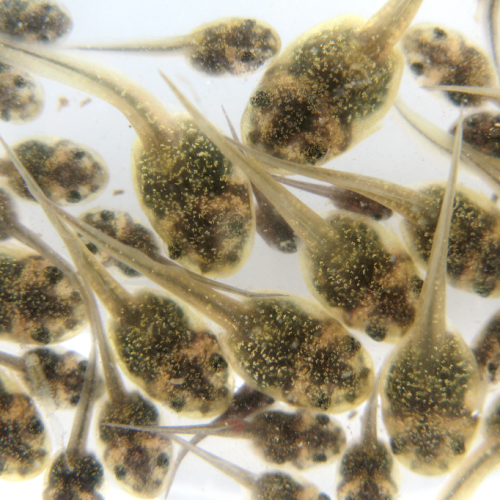
Photo CCs: Mouse pancreatic islet from Wikimedia Commons