The scientific breakthroughs just keep on coming hard and fast. At least in the realm of science, when asked what time period you’d like to live in, the answer is always the here and now.
If only the future was a possible option though, where we could see the true effects of the amazing innovations that are just starting to poke their heads up out of the bedrock that makes up the rules of the universe.
On that note, let’s jump to Stanford University where researchers in their Waymouth lab have accomplished the gene editing of a living mouse specimen. But also in a way that is temporary and not a permanent change, opening up a number of options for future use. Genetic vaccinations, anyone?
But before we go into all of that, first the field of gene therapy has to be examined and explained. Let’s start at the beginning.
A Historical Overview
Gene therapy, as miraculous as it may seem, is not new. It was first made a point of discussion among scientists in the 1970’s and first attempted in 1980. The attempt didn’t work, by the way, but that’s expected for early attempts. More research was conducted over the following decade, with a hard focus on alleviating congenital conditions.
In these beginning stages, the only options for gene therapy were to conduct them on the embryo itself so that it has the modified genes even from the beginning of its life. You may have heard of examples like these in the form of “three parent babies” where mitochondrial DNA was swapped for working copies.
The true successes of the field have only come to the forefront over the past decade, where treatments for a variety of conditions like leukemia have begun to be conducted on human patients.
So, that’s the history of it, but how does it work on the genetic scale of things?
Charged Problems
It’s as simple as you would think if you have a smidgen of understanding of genetics. Changing any of the genes changes the messenger RNA (mRNA) transcribed from it and that produces a different protein on the translation end. That’s just how any sort of altering of genes works, including from mutations.
That was an older form of gene therapy, however. Nowadays, the therapy focuses on directly changing the proteins being expressed without concern for the DNA and genes involved. This is normally done by directly sending in mRNA into the cell to be translated into proteins.
But this is a bit tricky. Messenger RNA has a number of negative charges on its surface (called anions) that overall makes it give off a negative electrical field that has difficulty getting into the cell membrane. This is because one of the main components of the membrane is the anionic phosphatidylserine and the two negative charges oppose each other.
Gene therapy researchers were able to get around this by using short interfering RNA (siRNA) that, while they still have a negative charge, have a much smaller charge overall and are able to slip through the cell membrane easier. Even this was not a great option though and there are many problems with it.
The Cart Revolution
The solution that was being investigated in the field was to use a positively charged transport mechanism of some sort, that would be able to shuttle the mRNA across the membrane and then release it.
And finally we are at the direct topic for today, since that’s exactly what the Stanford researchders did, they created that transport mechanism. They are known as charge-altering releasable transporters or CARTs for short. Cheeky naming scheme, I know.
It should be noted that CARTs aren’t the first attempt by scientists to make a positively charged (polycation) transport system. Those systems failed however because they kept their positive charge once inside the cell and that make it practically impossible for the mRNA to disengage, since the opposite charges were attracted to each other.
CARTs get around this limitation by converting to neutrally charged molecules (polyneutrals, which I don’t think is an actual word) once inside the membrane, releasing the mRNA. This change in charge also leads the CARTs to begin to biodegrade and are eventually removed from the cell.
Those Mice We Mentioned
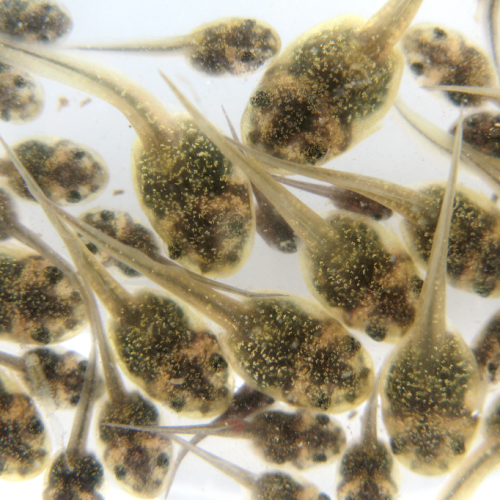
As you can determine, this is a huge advancement in gene therapy technology. To showcase the effectiveness of the method, the researchers used a glow in the dark protein from fireflies and inserted the mRNA instructions for it into a living mouse using CARTs.
And it worked perfectly. The mouse woke up afterward, no worse for wear, and now glowed in the dark. And because the mRNA doesn’t last forever, it has its own expiration date, the effects of the proteins it creates also don’t last forever. Making this a great way to have a long-term, but temporary gene therapy treatment for certain conditions.
Which brings us back to my prior statement on genetic vaccinations. With CARTs and particular mRNA, the researchers believe they can just have cells automatically begin producing antigens against diseases, rather than having them do it in response to a part of a virus or inactive version injected via vaccines.
And that doesn’t mean CARTs won’t have a use against lifelong conditions that require permanent changes. The scientists at Stanford are working on that too, where CARTs could transport an alternative version of instructions that would not degrade over time, continually producing proteins as desired.
New Era
As one of the co-authors of the paper put it, this sort of research is “part of a new era in medicine” and will likely completely change how gene therapy is conducted. Combine it with several other techniques in the works and you have a fully functional method to treat each and every genetic condition and give genetic protection against diseases.
Photo CCs: Mus mattheyi from Wikimedia Commons