Synthetic biology is complicated. When you’re building biological systems from the ground up, how could it not be? But the results are almost always something amazing, a real revolutionary accomplishment that wouldn’t be possible with any other field of science. The only other field that comes close is nanotechnology and mechanical systems are still somewhat behind the ability to create biological components that do the same thing.
The Importance of the Microbiome
Disease treatment is often based on the ability to sense complications ahead of time and begin countering the oncoming disease as soon as possible. This is especially true for more difficult and fatal disorders like cancer. But not all diseases give off clear, easily visible markers ahead of schedule or, if they do, they can often be misinterpreted to be something else entirely.
For a number of diseases, the state of the gut microbiome is key, since the bacteria, fungi, and archaea that live there are so important for the regulation of other bodily functions. Thus, any sudden change in the microbiome can be an indicator of other problems. Because of this, synthetic biology has had a long focus on developing bacteria that can act as sensors for certain chemicals that might paint a clearer picture of what disorder is forming.
Two chemicals in particular, thiosulfate and tetrathionate, are directly connected to the development of inflammation in the colon, commonly called colitis. Most causes of inflammation also lead to the conversion of thiosulfate into the latter chemical. The inflammation itself, in turn, can be connected to a variety of concerning diseases, including Crohn’s disease, ulcerative colitis, and more. Many of which may directly lead to colon cancer.
So, recognizing that these biological markers are converting into the other and building up can be of great importance in helping treat a person that will soon be suffering from one of these conditions. But what’s the best way to do that?
Creating Inflammation Sensors
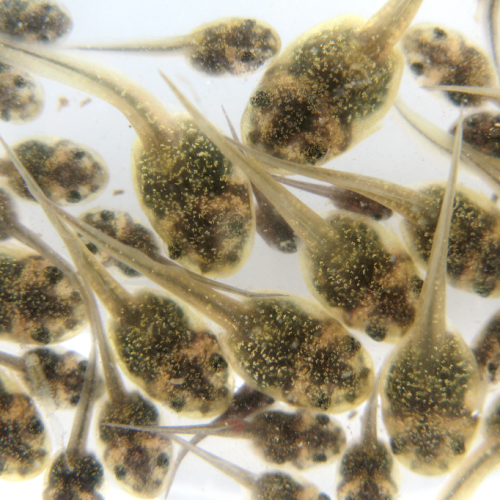
That’s where researchers from Rice University and the Baylor College of Medicine come into play. Their new experiments and testing have resulted in a strain of Escherichia coli (E. coli) that can sense the lack of thiosulfate in its surroundings, indicating the formation of tetrathionate leading to inflammation. Then, the activation of this sensor triggers a linked gene, Green Fluorescent Protein (GFP), and this causes the bacteria to glow green, which is easily detected in stool samples afterward.
The sensor itself is a two component system that was obtained already constructed from a marine bacteria called Shewanella halifaxensis. Some modification to their structure and expression were made within the genes and then the two separate components were encased in plasmids. The scientists had these plasmids be taken up and utilized by experimental E. coli, confirming their incorporation into the bacteria’s genome. This newly formed bacterial sensor was then tested in mice that were made to consume the bacteria and then were also injected with thiosulfate, tetrathionate, a combination of the two, and a control group without either.
A Variety Of Applications
The experiment was a success, having the bacteria light up to indicate the start of inflammation. The next step is to make further modifications to the sensor and the indicator, as GFP is not readily visible for the layperson. The hope is to add a gene for the production of a blue pigment that will be created by the bacteria, making its presence and activation completely clear. This would then allow the bacteria to be used in something akin to yogurt to test whether an inflammation flare-up is occurring.
Other sensor systems testing for other kinds of biomarkers should also be possible, opening the door to a world of genetically engineered bacteria for testing a wide range of conditions. At the very least, it would reduce or even outright eliminate the need for colonoscopy operations except for actual direct treatment.
Photo CCs: Diverse e Coli from Wikimedia Commons