When it comes to using CRISPR on a broad scale, different types of applications have to be utilized for different systems. If modifying bacterial genomes are the focus, then a viral vector to get the CRISPR complex into the cell is efficient enough for most purposes. But on multicellular organisms, there can be a number of problems with this method in addition to just a far higher failure rate of incorporation into the desired cells, the prime issue involving the host immune system that react to a viral invader and lowers success chances even further.
Delivery Action
It is because of this that so many other delivery mechanisms have been under investigation over the past few years, including a huge number of nanomaterials designed for the purpose. They have managed thus far to show a high efficiency in getting the CRISPR complex into the right cells, but not in timed and controlled activation of the gene editing process. Since, in many cases, there may be a certain time window or duration of activity that is needed for the CRISPR to begin its work, especially when it comes to the possibility of editing cancerous tumor cells.
There are a couple of options for controlled activation in modern science, but one of the methods having the best billing and research is photoresponsive molecules, essentially nanoparticles that respond when certain wavelengths of light reach them. Even within this specific class of biochemistry, there have been many forms that have been tried. Some better than others, depending on their individual chemical and structural alterations when exposed to such light. Those that rely on UV light have the potential to damage tissues, so only nanomolecules that can be combined with near infrared serve as a viable medical alternative.
Controlled Responsiveness
Back in 2015, particles of that nature were created in the form of lanthanide-doped upconversion nanoparticles (UCNPs) that respond to low energy infrared radiation that is capable of going into deeper tissue regions without harm. Now, a research team in China has taken those UCNPs to use as a delivery system for CRISPR-Cas9 for cancer therapy. The complex was anchored onto the UCNPs with a molecule that would be cleaved after exposure to the required light intensity, along with a polyethylenimine coating to help with membrane escape within the cell. The target gene to cut out was polo-like kinase 1, whose loss has been found to greatly slow tumor development and kill cells.
This method was first tested in isolated cell cultures, where it saw great success. The bigger step was to take the same system and apply it to a mouse subject, which they did. Mice with the type of cells that the guide RNA had been made to target in the Cas system were used and injection of the entire group of molecules into the mice intravenously. That helped show how the group would end up distributed throughout the body and was followed with direct intratumoral injections. The mice were then irradiated with the low energy light for 20 minutes every day to keep up activation of the CRISPR complex.
The two control groups, injection of salt water versus injection of the complex without irradiation, saw a huge growth in their tumors over the time period of 20 days. The experimental group, meanwhile, saw a gradual delay in growth over that time, only reaching a size 74% that of the control groups. Dissection of the tumors afterwards showed that cell density had greatly dropped in the experimental group and general cell apoptosis was seen. A histological look at major organs was also done to confirm that no toxic side effects had occurred from the injection and nothing of the sort was uncovered.
A Multi-Focused, Though Limited, Treatment
Thus, an effective method to delay and even destroy tumors if caught early enough has been developed, with the ability to regulate the activation of its systems whenever medical professionals deem is best. The primary downside that remains with this option is that direct injection into the tumors are needed, as a delivery mechanism that can target itself to the cancerous cells isn’t available for this method. So certain types of cancers will not be treatable in this way due to the inaccessible locations of growth.
Overall though, this seems like a worthwhile method of causing cancer cells to kill themselves through the lack of require cancer growth genes and may serve as a primary way to treat some forms of cancer. If combined with other medical technologies, a real cure without the need for chemotherapy may be possible. For now, further research in nanomedicine delivery is needed to better ferry the CRISPR complex to the desired cell locations.
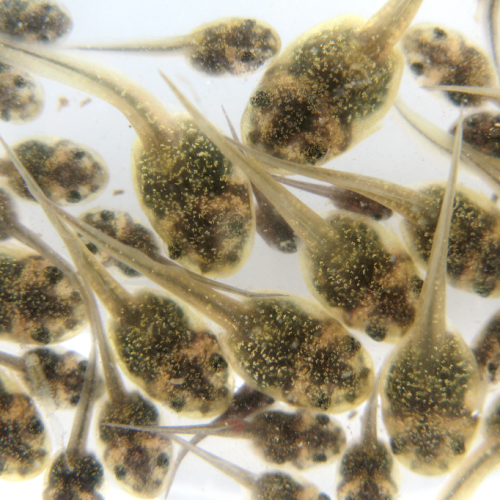
Photo CCs: Cancer cells (1) from Wikimedia Commons