Our nervous system directs most of our body’s mechanisms without us being away of it. Motor neurons are involved in moving parts of our body, sensory neurons give us each of our major secondary senses like our sense of pain or temperature, and interneurons connect all the other neurons together into a combined whole that communicates with the controlling master neurons in our brains. It is a complex, beautiful network that makes us able to do our everyday tasks as we live our lives.
But not everyone is so lucky. Accidents can happen and our nervous system can be sent out of control. This is especially so when it comes to spinal cord injuries, as the neurons there make up the central nervous system that branches out to the other parts of our body. When damaged, the resulting chaos can shut down entire limbs, resulting in paralysis. If the damage is too high up the spinal cord, it may even cause the neurons controlling our vital organs to fail, inevitably leading to death.
Sensory Regeneration
Finding ways to fix these broken neurological systems in such patients is a major field of study, though scientists have been going at it from many different avenues. The engineering side of things have been developing mechanical limbs and devices to replace the lost functionality that patients are experiencing.
Another field, however, one we’ve spoken about here on Bioscription before, seeks to correct the problem at its source. That field is regenerative medicine, the study of making new cells to replace those that have been damaged, to regenerate someone’s body to its original state. The primary version of this research has been on using stem cells and converting them into new motor neurons to replace those lost in the spinal cord and grant the patient the ability to walk or move their arms once more.
That area of regenerative medicine has seen huge advances and is reaching the point with modern technology that we may be able to solve for most paralysis conditions if we can treat them early enough after the incident that caused the injury. We may not be able to have complete cures, but at least some functionality should be possible to be reestablished.
But there is the opposing region to this that has seen much less focus, the topic of restoring sensory neurons and the interneurons that connect them to motor interactions. In a way, movement and sense of touch go together. Lacking the latter results in what is more or less a perpetual state of having an asleep limb, where it can be moved, but nothing can be felt from it. Therefore, it is clearly a necessity to restore sensory capabilities in addition to motor function.
Differentiating Stem Cells
Researchers at UCLA felt the same and decided to study how to transform stem cells into a more differentiated sensory interneuron state. These are the type of neurons that live in the spinal cord and connect the sensory neurons in the rest of the body to the brain. There are 6 different classes of sensory interneurons that are differentiated on the dorsal spinal cords. The scientists focused on being able to produce the first three kinds.
Dorsal interneuron 1s (dI1s) are involved in the sense of proprioception or the capability of sensing where your limbs are at any time while they are in motion. Then, dI3s help with touch-mediated motor responses, where touching something causes a instinctive motor reaction, such as touching something sharp. But, dI2s currently have an unknown function.
Using both human embryonic stem cells and induced pluripotent stem cells, the researchers went through the steps to induce differentiation. They hoped that by modifying the protocol normally used for making motor neurons, they would be able to convert to sensory interneurons instead. The first step was to culture the stem cells in a neural differentiation medium . This helps to direct their development toward neurological types of cells.
The second step was to add the signaling molecule, retinoic acid, that gives the cells the identity of being a part of the spinal cord neurons. The third step usually involves the addition of a molecule like purmorphamine that acts antagonistically to the normal Sonic Hedgehog signaling pathway for cell development. That is the normal final step to making motor neurons. But, since that wasn’t the goal here, the researchers tried something different.
Instead of purmorphamine, they added BMP4, a member of the bone morphogenic protein family that help to direct the activity of spinal cord neurons and that, without them, lab mice have been found to not be able to form those neurons. But this was found to not be effective toward forming sensory interneurons, because their development follows a different timeline than motor neurons. Thus, BMP4 needs to be applied at a different point in the process.
Multiple Methods For Multiple Cells
After looking at the expression levels of the stem cells and their genetic activation amounts in each stage of the protocol, they were able to determine that the BMP4 needed to be applied along with the retinoic acid in order to push the stem cells toward becoming dorsal sensory interneurons.
They were then able to create a set of dI1 and dI3 sensory interneuron cells at largely equivalent amounts, but it appeared that the BMP4 protocol was suppressing the formation of dI2 cells. However, with some alteration, they were able to make dI2 cells after following a new protocol not using BMP4. There would just need to be two separate methods for making the different cell types.
Interestingly, they found that the cell development from stem cells differed in separate species as compared to human stem cells. It appears that the differentiation process and formation of neuronal circuitry is genetically controlled in a contrasting manner and with a dissimilar timing sequence in different species.
Overall, they found no changes in the success of the protocol when using human embryonic stem cells or induced pluripotent stem cells. This contradicts a study published 7 years ago by other researchers, so confirmation of this fact may need to be undertaken by an independent group.
A Step Toward Regenerative Therapy
Either way, this study is the first step toward making replacement sensory neurons a reality for those suffering from paralysis and similar spinal cord injuries. The researchers hope to do further study into the transcriptomic changes during the protocol, along with the electrophysiological variance, in order to better understand what is happening within the stem cells when they differentiate into sensory interneurons.
But, regardless of ongoing experimentation, this is an important milestone leading to the potential use of this method in cellular replacement therapies in the future. It is yet another step toward finding a treatment for a set of debilitating conditions.
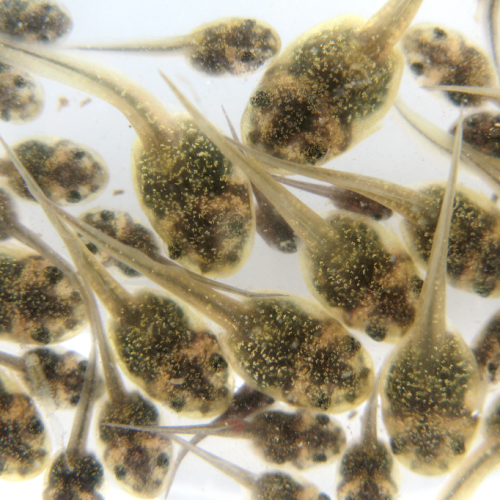
Photo CCs: Neuronal explosion from Wikimedia Commons