Drug resistant pathogens are an ongoing plague for the medical field and efforts to find original drugs and other solutions are slow going. The past few years, however, have seen some new scientific discoveries that might finally prove to be a more long-term option to help deal with such disease-causing offenders. These contemporary options though usually stray away from the topic of drugs and pharmaceuticals and look to other areas of research for answers. In this manner, while successful, they may also be avoiding the fundamental basics as well.
That is what researchers at Penn State University believe, at least. They realized that a lot of the research going on to deal with pathogens focuses solely on the already resistant types, completely ignoring the component of susceptible pathogens and their role in the microbiome environment. And that role appears to be significant and may completely change how drug resistance research is conducted.
Outbreak of Drug Resistance
Let’s start at the beginning though, with a little description of the way pathogens and drug resistance work. Generally, all pathogens, let’s stick with bacteria for this conversation, start off being susceptible to a new pharmaceutical drug. It targets some specific component of their metabolic processes or structure, thus killing them. Of course, not all cases will have every bacteria be susceptible, but that matters little at this point.
The drug takes time to get to and kill all of the target bacteria. During that period, the bacteria continue to divide and reproduce into new generations. Randomly during this generational process, there is a chance that one of the bacteria will obtain a mutation in the part of the genome coding for whatever structure or system is targeted by the drug. And, so long as this mutation isn’t deleterious enough to outright kill the bacteria, that results in the bacteria being resistant to the drug itself.
Continue on for many more generations and you suddenly have a population almost completely full of resistant bacteria, because those were the only ones to survive to this point. That is the process of how drug resistant pathogens form.
But a key thing to note is that this mutation, in order to make the pathogen resistant, also had to make its biological processes inefficient in some small part (sometimes in a large part). Therefore, in a direct competition without the drug involved, the susceptible pathogens without the mutation would win every time and out-compete the resistant ones.
Creating Forced Scarcity
This is why resistance gradually goes away in a population so long as the drug is no longer introduced. This provides an opportunity and the researchers at Penn State wanted to run an experiment to exploit that opportunity. The big question was, what if a resource scarcity was introduced to the pathogen population that made that competition between the two groups even more fierce?
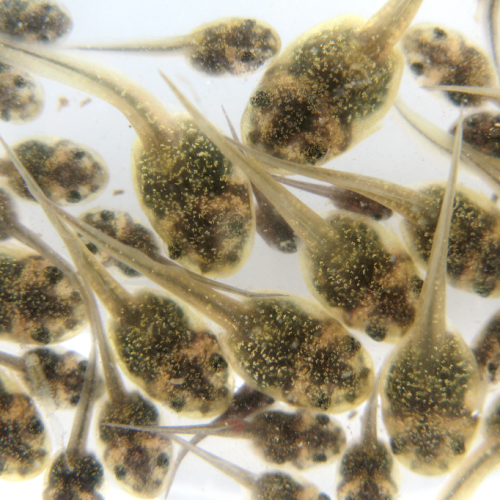
So they set up a test. Using a mouse model infected with a malaria pathogen, Plasmodium chabaudi, they introduced a drug to fight against this parasite. The drug they chose was pyrimethamine, which competitively inhibits certain enzymes in the parasites. Next, they identified the resource that the resistant parasites require to function, para-aminobenzoic acid (pABA), and they limited its availability by controlling the diet of the mice. This amplified the competition between the parasites susceptible to the drug and those resistant to it, with the former being more fit to compete for the resource.
Comparing two experimental groups, one where pABA was supplemented in the diet and another where it was limited, they found that the group with ample pABA had their parasite population rebound after drug treatment, now resistant to the drug in question. The other group had the exact opposite effect however, with the limited pABA resulting in the population plummeting and resistance not forming.
To confirm and test for any extraneous variables, they conducted another experiment where they compared mice infected with both susceptible and resistant parasites and a group infected with only resistant parasites. What they found was that, even under pABA-limited conditions, the group with only resistant parasites saw their population rebound and remain stable.
The Fundamentals
This confirmed that it was directly the competition between the two sets of pathogens that was causing the resistant pathogens to die out, even when using a pharmaceutical drug. Further testing showed that, while it may not be 100% effective in all mice tested, the resource limiting method did result in a reduction of resistant pathogens forming overall.
Going back to the basics to increase understanding of the fundamental components of how pathogen communities function is an extremely important task. Especially since most drug resistance research is done by only using resistant pathogens and completely neglecting the susceptibility element.
Now, hopefully this research will lead to a restructuring of how such studies are conducted and begin including resource scarcity as an additional tool to help extend the lifespan of pharmaceuticals and our ability to fight against the rise of drug resistant pathogens.
Photo CCs: Liver stage malaria parasite from Wikimedia Commons