Sometimes doctors are able to accomplish the most miraculous of surgeries using top of the line technology. Treatments with an incredibly low chance of success and with a high risk of death. Successes that likely will not be possible to do again in the near future, even with other patients with the same condition. That sort of story is what we’re talking about today.
Junctional epidermolysis bullosa (JEB) is probably one of the more horrible genetic diseases that you’ve never heard about. Approximately 7000 people worldwide have the condition and that is without considering the 40% that will end up dying in their first 10 years of life due to it. Let’s get into the details of what it is and what the genetics behind it are.
To start, let’s just say this bluntly. JEB is a genetic disorder that causes the outer layer of the skin to not be properly connected to the inner layers. It quite literally peels off without much force needing to be applied. Additionally, skin lesions are common and these, along with the exposed inner skin membrane, make sufferers of JEB prone to infection and various kinds of skin cancer.
Understanding Your Skin
Before we get to explaining the genes, let’s give a brief overview of the structure of the skin. The outermost layer of your skin, the epidermis, is almost entirely made up of specialized skin cells called keratinocytes. These are filtered throughout the five layers of the epidermis and the bottommost basal layer has ones referred to as basal keratinocytes. These are essentially the “stem cells” of this cell type and their division helps to replace the upper layers as they are sloughed off through daily activity.
Below this epidermal layer is a basement membrane and then the dermis and all of its layers. We don’t have to worry about those here, but that’s the general composition of the skin. The next thing to point out is that that basal level of the epidermis has special riveted structures that are used to bind the basement membrane to the epidermis above. These structures are called hemidesmosomes.
These bindings that connect the epidermis to the membrane and the lower dermis are of import here. Mutation in any of three different genes, named LAMA3, LAMB3 or LAMC2, can change the production of a protein called laminin-332. This is an essential protein that helps to keep the binding between hemidesmosomes and the different layers of skin. A significant number of cases involving such mutations result in death due to lacking laminin-332.
For those that do survive, their hemidesmosomes are very rudimentary in form or, in some cases, completely absent. This results in the epidermis lacking a proper connective binding to the lower layers and causes it to easily come off. Because this is a genetic disorder, there is currently no cure for the condition or even a direct method of producing new hemidesmosomes for the sufferer.
A Needed Treatment
But in June of 2015, doctors from Germany and Italy decided to try something different and sideways. Their patient was a 7-year-old child with a fairly severe case of JEB. The sores on his body had been getting worse and, six weeks before he was due to have an initial test done, his condition worsened due to several simultaneous infections. By the time that previous attempted fix had failed, the child had lost 80% of the epidermal layer on his body.
The ethics board and the child’s parents approved an experimental treatment involving gene therapy and stem cells. In September of the same year, a biopsy was performed to obtain a small sample of the child’s skin that remained and this was used to create a culture of the aforementioned keratinocyte stem cells. Next, a viral vector was used to transgenically introduce a working version of the LAMB3 gene that the child was missing.
The cell culture was then grown until 3 square feet of skin was available. This skin was grafted onto the child in three separate surgeries in October of 2015, November of 2015, and January of 2016. The skin was also used to test whether skin cultures grown on plastic sheets or on a fibrin substrate led to better engraftment and regeneration of the epidermis. Both were used on different parts of the child’s body and both saw success.
The Aftermath
A month after the last of the grafting surgeries, the doctors were able to confirm that the epidermis had properly grafted onto the lower layers and was regenerating. This included the skin growing to cover the previously exposed lesions and any leftover denuded (skinless) areas.
It has been 21 months since then and, after several repeated renewal cycles, the child’s epidermis appears to be the same as normally grown skin, including having the elasticity and resistance to mechanical stress of skin. Small biopsies taken at different points confirmed that the keratinocytes in the skin were only the transgenically transformed ones. The production of laminin 332 was also shown to be identical to that of someone without junctional epidermolysis bullosa.
The doctors took care to note at the end of the study that this was an exceptional situation. It required a child of the proper age and the surgeries conducted were massive and “aggressive”. In most cases, the patient would have died regardless. Thus, this sort of treatment cannot currently be said to be possible for any other patient with JEB without the same amount of risk and it would likely require them to be in the same near-death condition as the patient was in this case.
A Peek In The Door
However, the success of the grafted transgenic stem cells opens up the method in general as an option to help those with JEB (and other such conditions) over time and not as just a last resort. Skin symptoms could be treated as they arise by using a cultivated culture of the child’s cell taken from birth, thus reducing the risk of the children contracting infections or other side problems from the disorder.
This particular example of the treatment being done in such an aggressive, extensive manner may not be an advisable option for the future, but the method it represents is a huge step forward for gene therapy treatments and the use of skin grafts. The medical field will likely benefit greatly from this achievement and the lives of hundreds of children will be made the better for it.
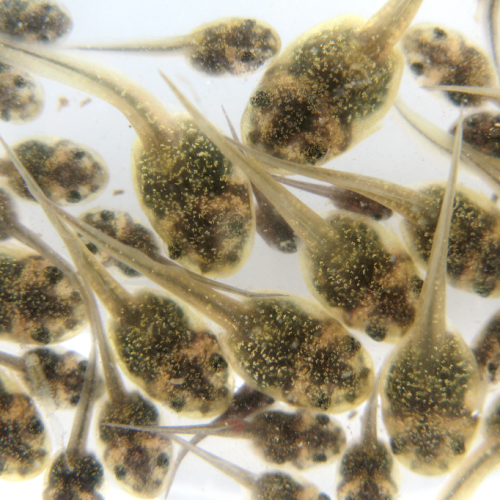
Photo CCs: Proliferative response induced by a tumor promoter in the epidermis of a wild-type mouse from Wikimedia Commons