The fight against the many forms of cancer has been a long and ongoing battle, with each different type requiring a novel and targeted solution to defeat. Generalized treatments have arisen over time, with the likes of CAR T-cell therapy, but there are still numerous hurdles depending on the cancer being dealt with. Before that can be explained, first we must discuss the aforementioned chimeric antigen receptor (CAR) T-cell therapy.
Breaking Immune Responses
Using biotechnological techniques, medical advances have allowed for the removal of some of a patient’s immune cells, genetic modification of them to express certain gene components that target receptors on the exterior of the particular cancer the patient is dealing with, and then reinsertion of those immune cells to begin the hunt to destroy cancerous host cells. It sounds pretty simple when explained like that, but it is the result of decades of research and experimentation to get us to where we are now. And, though still in a number of clinical trials, there is a huge amount of evidence that the therapy is effective against several kinds of cancer and can even persist in their immune response for up to 24 months.
However, there is a scenario where this is not true: when there is a form of cancer that creates large masses of tumors. The environment inside a tumor is quite different from the rest of the body. For one, the connection to the normal blood flow system is cut, meaning that it is difficult for any non-cancer cells to obtain nutrients while stuck inside such a mass. So for the engineered T-cells, this means their expansion and proliferation is suppressed and can lead to metabolic starvation, completely preventing their activity of cancer cell destruction. That is a problem.
For T-cells to proliferate properly, they require the necessary signaling molecules and cytokines to be provided that keep up their genetic response of division. This stimulation is cut off when inside a tumor mass and, without it, the T-cells lack the capability to overwhelm their foes. It is possible though to engineer the T-cells to also produce certain cytokines directly, such as an ongoing experiment with interleukin-15. That has been shown to be capable of keeping up proliferation rates in this very sort of situation. This was the proof of concept to show that engineering T-cells to make their own signals for proliferation is possible.
Cracking The Tumor
Jumping off from this point, researchers at the University of North Carolina at Chapel Hill started looking into how they could do even better than that ongoing experiment. What they found from other, separate projects is that IL-23 is a member of a group of cytokines known as STAT3s, which have been seen to have better results in those suffering from a particularly nasty form of leukemia. This cytokine is made up of two components, an alpha p19 and a beta p40 subunit.
What they uncovered and decided to test was that p40 appears to allow the T-cells to more directly control their proliferation without affecting surrounding cells. This prompted them to engineer those T-cells with their own p40 subunit production and they saw that this had an extremely enhanced anti-tumor capacity in mouse models. Not only did they have improved expansion abilities, they also lasted longer in the organ tissues and were shown to have direct tumor regression results as compared to engineered control CAR T-cells.
They were also able to see that these modified T-cells prompted the production of complete IL-23 within the tumors and allowed all the inserted cells to remain active with continued repression, all without spreading beyond the tumor itself and affecting the rest of the body. The effect appears to stay completely localized to the targeted tumor, which is good for preventing an overrun immune response elsewhere. The scientists also did a comparison of impact with IL-15 modified T-cells and IL-18, another known candidate for anti-tumor activity. This side by side conflict showed that the p40 subunit of IL-23 outperformed the other two by wide margins and not just in reducing existing tumors, but also regarding the safety factor of preventing outside negative effects on the patient’s tissues.
Research And Research Again
Previous to this research, there was a more controversial opinion on IL-23, as low dosages of its expression had potential inflammatory and tumor progression results. But the researchers here were able to show that at high levels of expression through modified T-cells, none of those side effects occur and the toxic secondary spread of cytokines is prevented. This is because the p40 subunits that help create a complete IL-23 molecule only enter production once the modified T-cell is activated upon encountering cancer cells, rather than being constantly active. So the secretion of this cytokine only ever targets the tumor cells themselves, restricting the location of its expression.
Further testing will need to be done to triple-check these facts in multiple models and clinical tests, but things look promising for this new version of CAR T-cell immunotherapy and our capability to fight against even more deadly cancers that cause tumor formation. Regardless though, this is a massive new strategy that can be employed against one of the most pernicious of human ailments and there should be high hopes for positive outcomes in the coming years. With every step, we come closer to eradicating all forms of cancer (and many other diseases besides) for good.
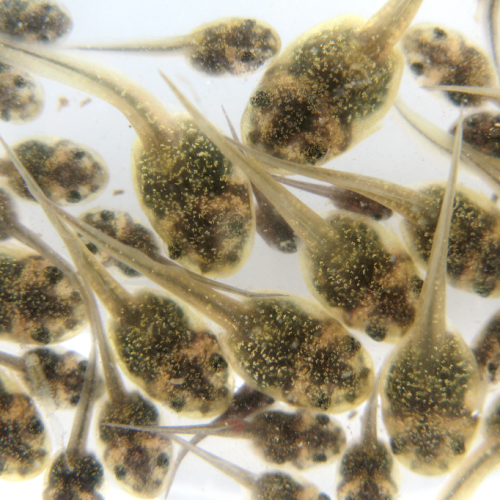
Photo CCs: 3D still showing tumor from Wikimedia Commons