The methods available to treat bacterial infections are many. But among those with any real and lasting effectiveness, their usage is limited. Antibiotics were once the Holy Grail of medicine to deal with devastating diseases that wiped out entire populations. With them, these suffering conditions were almost entirely wiped out and the populace began to learn how to live without the fear of most children dying at a young age. But, as is well known, the age of antibiotic cure-alls is ending and the time of antibiotic resistance is beginning to reach its peak. So, medical researchers are hard at work on all the other opportunities for dealing with bacteria that don’t require these specific groups of compounds.
The Medicine of Viruses
Phage therapy is one such alternative that has begun to see more extensive use over the past two decades.Bacteriophages are lifeforms that have crafted over evolutionary time a niche focused on using bacteria as their reproductive hosts, killing said host in the process. And since they are living beings as well, they actively engage in the selective pressures of finding ways around resistance against them, rather than being a static attack on bacteria like antibiotics are. This means that even the most feared multi-drug resistant bacterial strains have little to no protection against phages.
The primary downside to this treatment is that phages are highly specialized, having formed themselves to only target a particular host species. Therefore, to deal with certain bacteria, one also has to find and be able to cultivate a certain type of phage. Once that step is accomplished, however, it has been found that they can be altered fairly easily to give them variable methods of attack, so as to minimize any potential side effects on the human body while they are killing the bacteria. They can even be set up to synergistically interact with the human immune system to work together to wipe out the bacterial invasion.
With the right phage strain, the largest remaining issue is how to get them into the human body and to the right type of location and system that the bacteria are also attacking from. A large proportion of phage research has gone into finding new ways to do this very thing, as it is one of the inefficient areas of the therapy and, if improved, can drastically heighten the success rates of the treatment and the types of bacterial diseases that can be combated.
It is difficult and time consuming to produce modified phage, with many of them dying in this fabrication. For bacterial diseases of the lungs, such as the kinds that like to colonize those suffering from cystic fibrosis, there is currently no true delivery method of getting phage into the deep lung tissues. And, of course, getting any single treatment approved requires showing success in some sort of animal model, even though the phages may not translate well or at all to anything other than humans. This is one of the major problems this author has with the current approval setup by governments for medical trials.
Microparticles For A Micro World
Scientists at the Georgia Institute of Technology have been seeking a new method for just such a delivery system. Dry powder formulations has seen some positive benefits for effectiveness in recent years, but there lingers the issue of how to use such a powder to delivery living phages to the right spot. To do so would require a very carefully made powder indeed.
The engineering techniques they brought into play were used to make phage-loaded microparticles (phage-MPs), hollow molecular structures formed using water-oil-water emulsion to keep them stable. The bacteria being combated was the opportunistic pathogen Pseudomonas aeruginosa and several strains of phage against it were chosen for the experiment.
The microparticles were housed in a phage-containing solution, allowing them to be filled with the phage after incubation. Though they were filled in a different way than the usual method of them being inside the MPs. Instead, they cover the exterior in this method after the MPs are made, meaning no phage are lost due to solvent usage during MP fabrication from the prior ways other studies used. Three to five phages were contained on the MPs in order to reduce the likelihood of any possible bacterial resistance.
This delivery mechanism also reduces endotoxin production by the phage, thereby minimizing side impacts of their use, with the reduction bringing them down to 0.078 endotoxin units (EUs), far below the accepted FDA limit of 20 EU in treatments. The technique was first tested on petri dishes containing the bacteria to which the phage-MPs were applied. The P. aeruginosa were modified to express green fluorescent protein (GFP) to identify their living location on the plates.
A Complete Victory
After 16 hours of co-incubation, large patches of non-fluorescence showed where the phage had successfully killed off the bacteria, while the control group MPs without a phage coating had no deaths. These zones were also far larger than the applied MP area, showing that the phage were able to spread and extend to other bacteria in the dishes. The same test was done using synthetic sputum to mimic the environment of an animal lung and the bacteria and phages were applied at the same time. There was no visible growth of bacteria after application, showing that the phages were able to both control and wipe them out. A further test showed the phage are also able to get past the protective biofilms of the bacteria that they make under environmental emergencies.
The dry powder formulations were also seen to have a large burst of phages initially, with slow release for two weeks after, the perfect way to allow consistent application and treatment against the bacteria. The final experiment involved using mice infected with the bacteria. A control test using just phage-MPs showed no negative effects on the mice or their lungs after application. Fluorescent phage-MPs also showed that they were only localized to the lungs and nowhere else in the body, as desired. The control using free form phages without microparticles revealed how the dry powder still didn’t allow them to be properly applied, with no major phage levels detected in those mouse lungs, proving that the MPs as a transport vector were required.
When tested on mice infected with P. aeruginosa, the bacterial count dropped by an entire order of magnitude and 100% of the mice survived their pneumonia, while the untreated control group only had 13% survive. For mice with a cystic fibrosis genetic mutation, the same test saw their bacterial counts drop by three orders of magnitude, approaching the limit of what could be detected. The phage-MPs also saw the same effectiveness against multiple strains of the bacteria, meaning that even genetic variance in a population wasn’t enough to defend against them.
A last point of importance is that when testing against a mouse group exposed to phage-MPs long before being infected and later treated, there was no reduction in effect and no antibodies against the phages seemed to develop. So there is likely no performance loss to the treatment if used multiple times.
The New Antibiotics
As a conclusion, the researchers were able to engineer specialized biomaterials made of microparticles that, when coated with bacteriophages, were highly effective at reducing bacterial counts for lung-related diseases, including those resulting from the lowered immune system responses of cystic fibrosis. These phage-MPs are stable and can be stored for a fair amount of time with no loss in phage amounts and can be administered through simple inhalation, meaning younger patients can be treated with less complications.
For lung-related diseases, and likely for broader conditions at large in the medical community, this breakthrough might serve as a major way to allow phage therapy to become more common and used in replacement of or as a sought after alternative to antibiotics. The number of lives this should be able to save in the long run is likely incalculable.
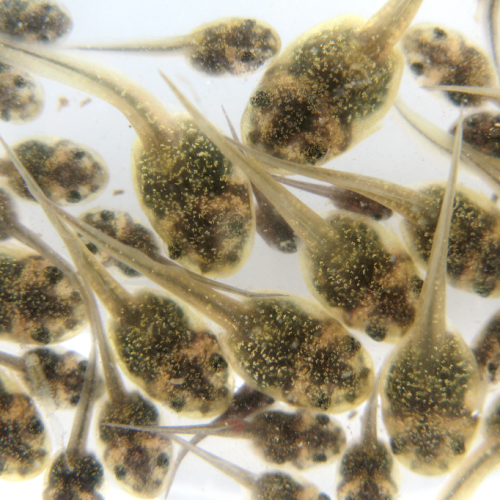
Photo CCs: Phage from Wikimedia Commons