When severe injuries occur, there can often be damage to skin, tissues, and organs. Depending on the extent of that damage, replacements can often be required. It has only been in recent decades that medical technologies have advanced far enough for things like skin grafts and organ replacements to have become viable and at a high enough success rate to be feasible. We are even at the point of growing skin and organs from a patient’s very own cells in order to reduce any risk of rejection of the replacements.
The Problem With Blood Vessels
However, there has always been one additional factor that has proven difficult to replace and that is needed for all cells in the body. Blood vessels and the oxygenating liquid they contain are small enough to require delicate formation, but extensive enough that production of them is of a magnitude that generally prevents individual patient treatment plans. The use of large-scale tissue grafts simultaneously requires the inclusion of some sort of vascular network, as diffusion isn’t capable of allowing nutrients and oxygen to enter into the cells in the middle of such thick tissues. This means that transportation via vessels is necessary.
Past research in this area has split into two varieties of somewhat success. Patterned vascular networks are created via the molding of a biomaterial into the correct shape and density and then allowing the patient’s endothelial (cells that line the interior of blood vessels) to invade the biomaterial’s form. The prime issue with this method is that the patterns needed to ensure the material doesn’t break or crack or deform in some manner often results in vessels set up in straight lines. These formulaic states don’t much match real living organisms and can cause cells to be grouped in strange ways, as cells are not all the same size and don’t remain in rigid shapes.
The alternative is a self-assembling system that begins with adding those same cells next to the biomaterial and allowing them to multiply and invade it. This process results in the endothelial cells creating natural lumen spaces for the blood vessels and creates the desired network in a real format. The main benefit of this option besides that is the process mimics the natural growth of such vascular systems in living organisms as they develop. The downside here though is the tendency for the cells to constrict and reduce their overall area, meaning only small areas of vascular tissue can actually be produced. Furthermore, these natural systems don’t tend to be stable outside of a body and break down in just a few days.
Producing The Perfect Vasculature
Researchers at the University of Delaware were studying this issue and aimed to devise a simple, scalable system using commonly available cells that can be made to produce vascular tissue for better study and medical testing. In that light, they began with human umbilical vein endothelial cells (HUVECs), an easily obtained cell type from discarded umbilical cords, and rat tail collagen as the biomaterial for development of the vessels. Multiple culture conditions were tested to determine the best growth and development state for the cells in this particular biomaterial.
What they found is that there appears to be a certain “sweet spot” where the amount of cells is high enough and the density of the collagen is just right. Too low a number of cells in high density collagen results in the cells not being able to proliferate properly and they often die off. The opposite scenario, of high cell amounts and low collagen density, always results in contraction of the tissue within 24 to 48 hours. But the just right density for both caused the formation of a working three-dimensional network that spanned the entire volume of the available collagen.
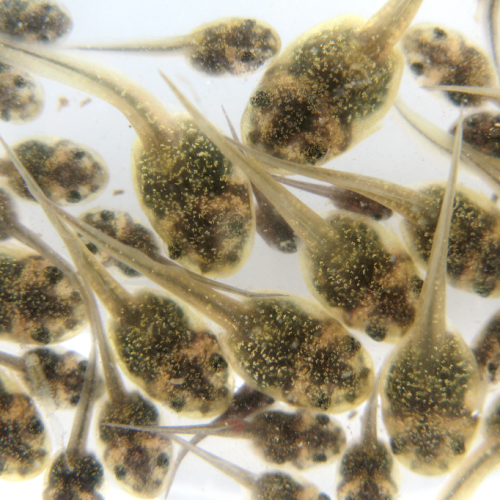
This successful culture was repeated in multiple forms of testing and perfusion with microbeads and dyes to observe the internal structures, showing that both large and small vessels had formed and created an interconnected network. Additionally, the vascular mats maintained cellular stability for upwards of 21 days after formation, more than long enough for both testing and possible medical usage. Necrosis of the tissue would largely not be a concern thanks to this so long as the tissue was developed a week or two ahead of any procedures.
Their experiment also allowed the researchers to begin getting a grasp on how the starting conditions result in varying morphologies of the vascularization, as would be needed for different types of organs and muscle tissues. They were also able to confirm oxygen penetration of the tissues in all forms and that the lumen of the vessels are able to support the flow of fluid through them without rupture.
A Research Tool And Possibly More
For now, especially as they were using rat collagen as their biomaterial, this invention only serves as an experimental tool for researching the ways that vascularized tissues develop and how to form them into the right shapes and densities at the desired sizes. It could also serve as a way to follow tumor growth, the impact environmental toxins have on vascular tissues, and any number of other diseases that affect blood vessels and the cells that make them up.
Improvements still need to be made in the future though. The current system has random sizing of the vessels, meaning they don’t represent a true network connecting arteries to capillaries to veins. The cell type used from umbilical cords also does not represent the far vaster collection of cells that are involved in vascular tissues across the body. So, while the system has great potential for future usage in science and medicine, this is merely the first step toward that and more complexity in design will be eventually required.
Photo CCs: Vessels (248 18) Cross-section from Wikimedia Commons